On this page Skip this page navigation
- Introduction
- Ontario’s Immediate COVID‑19 Health Response
- Protecting People’s Health during the Second Wave
- Protecting Our Loved Ones in Long-Term Care Homes
- Supporting People Suffering from Mental Health and Addictions Challenges
- Continuing the Commitment to a Strong Health Care System
- Protecting Workplaces
- Building an Emergency Volunteer Unit
Introduction
Above all else, COVID‑19 is a health crisis. As Premier Ford has promised, the government will do whatever it takes to protect the people of Ontario from this deadly virus.
To support this commitment, in March Ontario’s Action Plan: Responding to COVID‑19 quickly made $3.3 billion available in additional resources to ensure our health care heroes had what they needed to protect the people of Ontario in the face of the pandemic. This flexibility was key to the government’s strategy. Being nimble and responsive as the crisis unfolded proved to be a critical advantage that helped control the spread of the virus and ultimately saved lives.
Our government has been working through the summer to develop a plan for this exact moment. It’s the most robust and extensive plan anywhere in the entire country. This is a plan informed by the best medical advice and science, informed by Ontario’s Chief Medical Officer of Health. I want everyone to know we have every single measure in place. We’re taking every step. We’re sparing no expense to protect the health and safety of everyone.
Honourable Doug Ford
Premier of Ontario
This funding allowed the Province to respond in a meaningful and robust way, which included supporting 141 hospital and health care facilities, and operating 162 assessment centres. From the onset of the COVID‑19 pandemic, the Province has taken action to ramp up testing to enhance and expand efforts to test, trace and isolate new cases of COVID‑19. Since March 2020, the government has increased testing capacity more than tenfold, with 4.75 million tests conducted as of mid-October. Ontario continues to lead the country in both the number of tests completed and daily testing capacity.
An additional $100 million was also provided to public health units and $170 million for community capacity, home care and Telehealth Ontario to help the sectors respond to the first wave of COVID‑19. The government also purchased nearly $1.1 billion in personal protective equipment (PPE) and other critical supplies to protect our health care workers, patients, and people across the province.
With this investment, Ontario successfully navigated the first wave of the pandemic. But as we are also seeing in other jurisdictions around the world, Ontario is now dealing with a second wave of COVID‑19. And despite our collective efforts to avert it, the reality is that we must be prepared for future waves for the foreseeable future.
Building on the $7.7 billion in investments announced in the 2020–21 First Quarter Finances as part of the updated Ontario’s Action Plan: Responding to COVID‑19, Ontario has put forward a robust plan to protect people in the second wave and beyond. This Budget confirms total 2020–21 investments of $8.3 billion, $600 million more than reported in the 2020–21 First Quarter Finances. This will ensure that the necessary health resources are in place to protect people across the province. There is $0.6 billion remaining in dedicated health contingencies this year to maintain the flexibility that is essential to respond to emerging health needs.
The 2020–21 spending includes $2.8 billion to support the Province’s Fall Preparedness Plan for Health, Long-Term Care and Education (Fall Preparedness Plan), which includes additional funding to support hospital beds, address the surgical backlog and purchase additional influenza vaccines. The Province is investing $1.4 billion to expand COVID‑19 testing and ramp up case and contact management, while supporting COVID‑19 testing at pharmacies and in communities. Ontario has invested $351 million to create over 2,250 hospital beds to give the system capacity to address COVID‑19 surges in this second wave.
An additional $4 billion in 2021–22 and $2 billion in 2022–23 is being provided in flexible funding to help the health sector address its changing needs as part of the response to COVID‑19.
With the ongoing spread of COVID‑19, the continued threat to our loved ones in long-term care looms large over everyone in the province. To protect loved ones in long-term care from a second wave, and to address long standing issues in the system, Ontario is providing over half a billion dollars to enable necessary renovations and measures to improve infection prevention and control, allow for the purchase of more personal protective equipment (PPE), and to build a strong health care workforce.
The government is committed to improving the delivery of long-term care services. This is why the Province will protect residents of long-term homes by increasing average daily direct care per resident to four hours a day over a four-year period. This will help ensure resident care needs are being met and that residents have a higher quality of life.
These significant resources, along with public health measures implemented based on expert advice, helped Ontario emerge from the first wave. They will be just as essential moving forward. But ultimately, it will be the Ontario Spirit — which includes the hard work and sacrifice of our health care professionals, not to mention the responsible, respectful behaviour of our citizens — that will help defeat COVID‑19 once and for all.
Ontario’s Immediate COVID‑19 Health Response
The government responded quickly to respond to the COVID‑19 outbreak, with Ontario’s Action Plan: Responding to COVID‑19, including an immediate investment of $3.3 billion to protect people and equip Ontario’s health care professionals with the resources they need. The Action Plan also provided a dedicated $1.0 billion health sector contingency fund for any emerging needs to support the Province’s timely response to the pandemic.
Highlights of the government’s actions to maintain public health measures include:
- Established comprehensive testing across the province through a provincial lab network, assessment centres and mobile testing. Testing capacity increased more than tenfold, with 4.75 million tests conducted as of mid-October;
- Provided hundreds of additional contact tracers to support public health units in contact tracing through an agreement with the federal government;
- Launched COVID Alert, the country’s made-in-Ontario exposure notification app; and
- Launched a robust public awareness campaign to educate the public on how to keep themselves and their families safe, promoting compliance with public health measures (e.g., physical distancing, widespread use of face coverings).
Highlights of the government’s actions to quickly identify, manage and prevent outbreaks:
- Developed a COVID‑19 surveillance strategy to monitor the disease and detect cases and outbreaks in a timely manner, including in priority settings such as long-term care homes;
- Launched a new case and contact management system, customized for Ontario, to improve data quality and timeliness — implemented across 31 of 34 health units;
- Established a Rapid Response Table comprised of public health experts, to help address outbreaks and support public health units in outbreak planning and response;
- Established regional integrated planning and refinement of outbreak protocols;
- Supported deployment of hospital and other partner infection prevention and control (IPAC) resources to support long-term care homes;
- Continued implementation of the COVID‑19 Action Plan for Vulnerable People to better protect those living in high risk congregate care settings including homes serving those with developmental disabilities, shelters for survivors of gender-based violence and human trafficking, and children’s residential settings; and
- Piloted a project by Toronto Public Health for people who cannot self-isolate in their family homes.
Highlights of the government’s actions to prepare for surges in COVID‑19 cases:
- Provided virtual nursing and rehab home care services for patients, with over 240,000 visits since the COVID‑19 outbreak began;
- Supported more than 39,000 people in accessing virtual mental health supports available provincially through the government’s investment of $26.75 million in emergency mental health and addictions funding;
- Expanded integrated models of care to support patients transitioning from hospital to home or the community, with over 20,000 patients being served in 2020–21;
- Provided virtual check-ins through community-based service providers for vulnerable home care clients — many of them seniors — who have been housebound during the pandemic; and
- At the height of the first wave, added 1,035 acute care beds and 1,492 critical care beds and took steps to ensure hospitals have the staff available to care for a sudden surge in patients.
Highlights of the government’s actions to expand digital health and virtual services:
- Ensured the continuity of patient care with enhanced access to virtual care — done through the creation of temporary fee schedule codes that insured physician phone and video patient visits under OHIP and fee codes for virtual care visits; and
- Took a digital first approach to modernizing the health care system, including investments to enable more physicians to conduct virtual care visits with their patients using digital channels. This also includes providing new and improved digital health solutions to frontline care personnel, so that they can rapidly and securely access a patient’s health records.
Highlights of the government’s actions to recruit, retain, train and support health care workers, families and caregivers:
- Implemented a health workforce matching portal that made over 1,100 matches for over 1,000 employers across the health system, including 650 matches for long-term care homes; and
- Supported stability in key sectors and recognized the efforts of eligible frontline workers during the pandemic by providing a temporary pandemic pay increase of $4 per hour for work performed from April 24, 2020 to August 13, 2020.
These measures helped protect the health of the people of Ontario and reduced the spread of COVID‑19. Throughout the pandemic, the government has continued to work with Ontario Health, Public Health Units, the hospital sector, and other levels of government to respond to outbreaks and prepare for future waves.
Protecting People’s Health during the Second Wave
The government is responding to future waves of COVID‑19 by investing additional funding in the health care sector, including $2.8 billion to support the province in its second COVID‑19 wave. The government’s Fall Preparedness Plan for Health, Long-Term Care and Education (Fall Preparedness Plan) is built on six pillars:
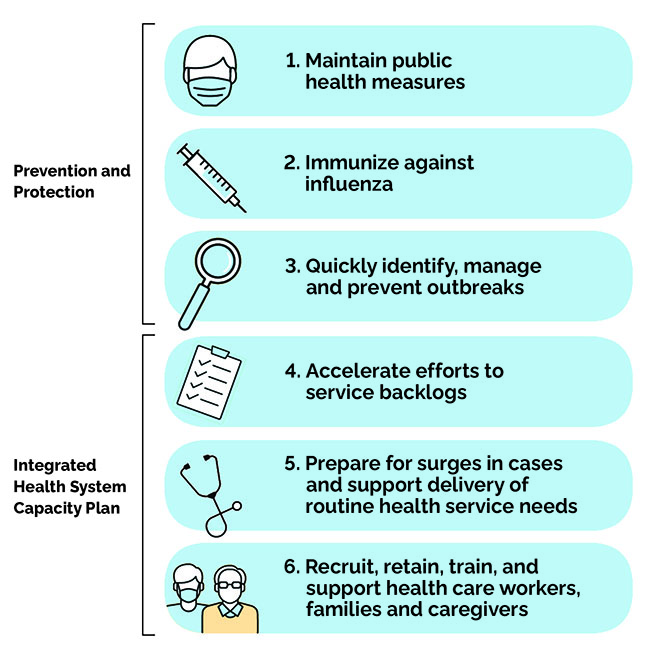
1. Maintaining Strong Public Health Measures, including Continued Expansion of Testing and Case and Contact Management
Testing, tracing and isolating COVID‑19 cases remains an effective measure to identify and contain the pandemic and is a key pillar in the government’s Fall Preparedness Plan. This is why the government is investing $1.4 billion to expand COVID‑19 testing and ramp up case and contact management.
This will support the operation of assessment centres across Ontario, ensuring these centres have adequate staffing and supplies. Assessment centres and mobile testing have played a critical role in helping identify new COVID‑19 cases during the initial wave of the pandemic. This additional funding will support assessment centres that will evaluate individuals who are experiencing COVID‑19 symptoms, vulnerable populations and those who have had known contact with a confirmed case. Pharmacy testing has been introduced for asymptomatic individuals, which will increase overall provincial testing capacity.
From the onset of the COVID‑19 pandemic, the Province has taken action to ramp up testing to enhance and expand efforts to test, trace and isolate new cases of COVID‑19. Since March 2020, the government has increased testing capacity more than tenfold, with 4.75 million tests conducted as of mid-October. Ontario continues to lead the country in both the number of tests completed and daily testing capacity.

2. Implementing the Largest Flu Immunization Campaign in Ontario's History
The second wave of COVID‑19 is overlapping with Ontario’s influenza season. The Province has committed to spending $70 million to purchase 5.1 million doses of the influenza vaccine. This represents the largest flu vaccine campaign in Ontario’s history and is one of the pillars of the government’s Fall Preparedness Plan. More high-dose vaccines have also been purchased to protect the most vulnerable. The Province is prioritizing early distribution of the flu vaccine for vulnerable populations in long-term care homes, hospitals and retirement homes. In addition, the Province is making it easier for seniors to receive increased orders of high-dose flu vaccines by making them available at participating pharmacies, as well as primary care providers and public health units.
The influenza vaccine will help protect the people of Ontario and reduce the number of visits to emergency departments, doctor’s offices and hospitalization, which will help maintain capacity in the health care system.
3. Identifying, Managing and Preventing COVID‑19 Outbreaks
Quickly identifying, managing and preventing outbreaks is one of the key pillars to the government’s Fall Preparedness Plan. Quick and effective management of outbreaks remains an integral tool in stopping the spread of COVID‑19. This is in addition to the government’s COVID‑19 Action Plan: Protecting Vulnerable Ontarians and COVID‑19 Action Plan: Long-Term Care Homes.
Strengthening Infection Prevention and Control Expertise
The first wave of the pandemic saw COVID‑19 outbreaks in hospitals, long-term care homes, retirement homes and other congregate care settings, demonstrating the need for strong infection prevention and control (IPAC) practices and policies. That is why the government has made significant investments to increase capacity in IPAC. This is part of the Province’s coordinated approach to managing COVID‑19 in congregate settings to ensure there are sufficient resources in place to better prepare for and avoid outbreaks in future waves of the pandemic.
Infection prevention and control remain priorities as outbreaks need to be quickly identified and contained. Hospitals and other IPAC professionals continue to support long-term care homes by providing infection prevention and control expertise. This is why the government is investing a total of $60 million to support IPAC measures in the health sector. The government has announced the appointment of Dr. Dirk Huyer as the Coordinator of Provincial Outbreak Response to work collaboratively with all ministries, the Chief Medical Officer of Health and public health units to prevent, minimize and manage outbreaks including those in schools, long-term care homes, retirement homes, child care centres, farms and hospitals.
Local networks of IPAC expertise are being developed from across the health system to enhance IPAC practices in community based, congregate living settings. These settings include long-term care homes, retirement homes, residential settings for adults and children, shelters and supportive housing.
Through a new, provincewide network, congregate living settings will be able to quickly access IPAC expertise, collaborative assistance and advice, guidance and direct support on IPAC practices for both prevention and response.
4. Accelerating Efforts to Reduce Surgical Backlogs
As the pandemic was emerging, hospitals were directed by Ontario’s Chief Medical Officer of Health to stop or reduce scheduled surgeries and procedures to minimal levels. This ensured hospitals had the capacity to treat patients and to help reduce the spread of the virus, but this created a backlog of over 180,000 surgeries and 380,000 diagnostic imaging scans. On May 26, 2020, hospitals were allowed to gradually restart all deferred scheduled surgeries.
The Province is investing $283.7 million to address this backlog while ensuring hospitals have the capacity to manage COVID‑19 and the influenza season. The Province’s investment will enable hospitals and Independent Health Facilities to address wait times by performing over 60,000 surgeries including cancer, cardiac, orthopedics and cataract surgery.
5. Preparing for Surges in COVID‑19 Cases

The government has made additional changes to reduce pressure on hospitals to ensure the broader health care system can respond to surges in COVID‑19 cases and the influenza season by expanding access to home and community care services. This includes freeing up hospital beds by providing up to 850 alternate level of care (ALC) patients with home and community care. These patients will receive, on average, seven to nine hours of personal support services and one-and-a-half to two hours of nursing care per patient per day in a home or community setting.
The government is also expanding existing community paramedicine programs or creating new ones to support ALC and complex patients in the home and community setting. The expanded programs will provide some patients who are waiting for a long-term care bed with additional support and care provided by paramedics.
Expanded community paramedicine will support the government’s strategy to free up beds and will allow hospitals to treat more severe COVID‑19 patients. This will also help alleviate pressures on long-term care homes as beds are being reduced as multi-bed rooms are being eliminated to control the spread of COVID‑19.
Ensuring Hospitals have Bed and Staff Capacity for a Second Wave
The Ontario government is proceeding with its $2.8 billion COVID‑19 Fall Preparedness Plan by investing $116.5 million to add up to 766 additional beds in hospitals and alternate health facilities across the province. Making more beds available will help reduce surgical backlogs and improve access to care during COVID‑19.
This is in addition to the 139 critical care beds and 1,349 hospital beds already announced as part of the Fall Preparedness Plan, bringing the total new beds to more than 2,250 in hospitals and alternate health facilities across the province.
Beds are being added across the province to help address the surgical backlog and ensure hospitals have enough beds to treat severe COVID‑19 patients, particularly in COVID‑19 hot spots. Beds are also being added to transition alternate level of care patients from the hospital to transitional health care settings, which will help alleviate the capacity pressure in hospitals. That is why the government is investing $351 million to add more than 2,250 beds across the province in response to the COVID‑19 outbreak.
6. Recruiting, Retaining, Training and Supporting Health Care Workers
As part of the Province’s COVID‑19 Fall Preparedness Plan for Health, Long-Term Care and Education, in preparing for future waves of COVID‑19, the Province is investing $52.5 million to recruit, retain and support over 3,700 more frontline health care workers such as nurses and personal support workers (PSWs). This investment aims to ensure Ontario’s health care system can meet any surge in demand, while continuing to provide safe and high-quality care for patients and long-term care residents.
Supporting Workplace Stability with Temporary COVID‑19 Pandemic Pay
The government supported stability in key sectors and recognized the efforts of eligible frontline workers during the pandemic by providing a temporary pandemic pay increase of $4 per hour for work performed from April 24, 2020 to August 13, 2020. Eligible workers who worked at least 100 hours in a designated four-week period were also eligible for a lump sum payment of $250 for that period. In Ontario, eligible employees who worked an average of 40 hours per week received about $3,500 in additional compensation.
More than 375,000 workers in health, long-term care, retirement homes, social services and corrections were eligible for temporary pandemic pay. Together with the federal government, Ontario made over $1.5 billion available for temporary COVID‑19 pandemic pay.
Protecting Frontline Health Care Workers
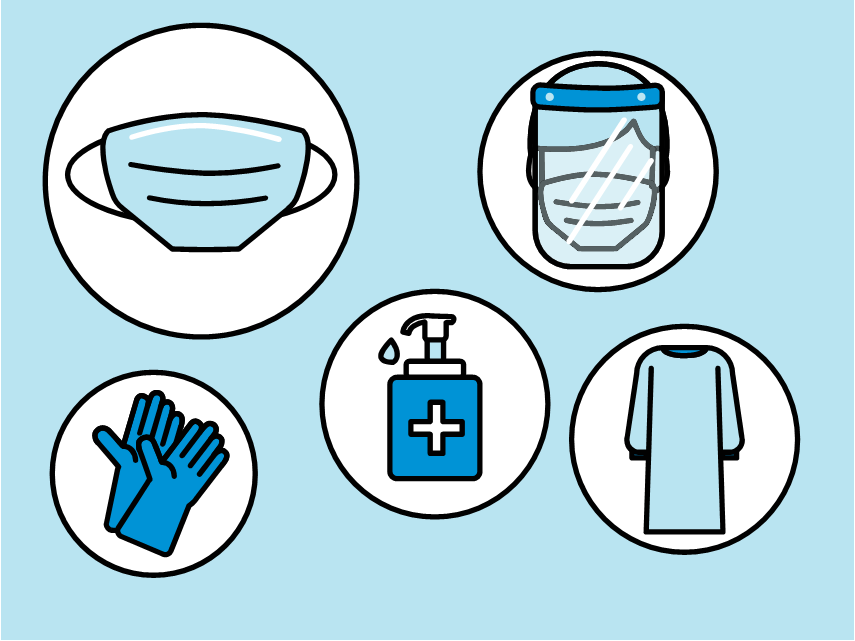
Since the start of the COVID‑19 outbreak, there has been an urgent need to procure personal protective equipment (PPE) and critical supplies to protect health care workers, patients and frontline staff in other sectors.
That is why the government has spent nearly $1.1 billion to ensure PPE and critical supplies are in the hands of Ontario’s health care professionals and other frontline workers. This investment has purchased nearly 300 million masks, 900 million gloves, 50 million gowns and over 6 million face shields.
Steps have also been taken to ensure the government can respond to increasing demands for these essential supplies. At the onset of the pandemic, the government took immediate steps to centralize procurement to ensure necessary access to PPE and critical supplies. This included developing robust modelling efforts and forecasting capacity to identify supply needs. Modelling efforts are also being used to inform how to best allocate and distribute the PPE across the province, including future decisions to purchase additional supplies.
With heightened global competition for critical supplies, the Province also invested in Ontario companies to begin domestic production.
Protecting Our Loved Ones in Long-Term Care Homes
There have been long-standing challenges in the long-term care system resulting from the inaction by successive governments. Rising complexity of care, staffing shortages and high daily care needs of residents are some of the key challenges faced by the long-term care sector. In addition, there were only 611 long-term care beds built across the province between 2011 and 2018, less than one bed per home. This lack of development has resulted in more than 38,000 people on the waitlist to access a long-term care bed.
The government is addressing these challenges to ensure the long-term care system is safe and responsive to the needs of the people of Ontario. For example, the government is developing a comprehensive staffing strategy based on advice of an external Long-Term Care Staffing Study Advisory Group, improving resident safety by implementing the recommendations of the Public Inquiry into Long-Term Care Homes and accelerating the construction of urgently needed long-term care beds through a modernized funding model.
The COVID‑19 outbreak was unprecedented and further heightened the systemic challenges already existing across the long-term care sector. Action was long overdue, and the government took immediate steps to keep the people of Ontario safe. Through the COVID‑19 Action Plan for Protecting Long-Term Care Homes, the Province used every tool available to respond to the COVID‑19 outbreak, such as providing emergency funding, staffing support and expanded testing, along with direction and guidance on outbreak management and infection prevention and control.
Supporting a Timely Response to the COVID‑19 Outbreak
The government is working to ensure that loved ones in long-term care are protected as COVID‑19 continues to unfold. In addition to the $243 million in support immediately provided to long-term care homes in March for emergency capacity and virus containment measures, the government is providing close to an additional $540 million in new funding to protect residents, caregivers and staff in long-term care homes from future surges of COVID‑19, for a total of $783 million. This includes:
- $405 million to help homes continue prevention and containment of COVID‑19 including enhanced screening, staffing supports and purchasing additional supplies and PPE;
- $61.4 million for minor capital repairs and renovations in homes to improve infection prevention and control;
- $40 million to help stabilize the homes as they transition to lower occupancy rooms, to stop admissions of third and fourth residents to larger rooms;
- $30 million to allow long-term care homes to hire more infection prevention and control staff and train new and existing staff; and
- $2.8 million to extend the High Wage Transition Fund to ensure that gaps in long-term care staffing can continue to be addressed during COVID‑19.
Long-Term Care Staffing Strategy — Increasing Hours of Care

While the challenges are longstanding and complex, the government is acting now to improve the quality of care for our loved ones in long-term care. This includes a commitment to addressing these challenges, including chronically overworked staff, a lack of full-time jobs, and poor perception of long-term care homes as a career destination. These challenges came into sharp focus during the first wave of COVID‑19.
The government is committed to protecting the most vulnerable people of Ontario and plans to increase average daily direct care per resident to four hours a day, making Ontario the first in Canada to commit to this level of care. This action will help ensure resident care needs are being better met and that residents have a higher quality of life. While it will take four years to fully implement this transformative change, the government recognizes the urgency of improving resident care quickly. The increases will be phased in over time.
The Province’s ambitious plan will require significant changes in the long-term care sector and the government is committed to working with its partners throughout its implementation over the next four years. The complexity and breadth of partnerships that will be required is extensive and requires collaboration with labour partners, care providers and training providers. While work is already underway, this new plan will require significant planning and coordination given the scope of unprecedented change that it will represent when it comes to resident care. For example, tens of thousands of new staff will need to be trained and recruited.
To provide residents with more direct care, there needs to be a sufficient pool of personal support workers (PSWs), registered practical nurses and registered nurses, to fill tens of thousands of new positions. The government is moving quickly to create new, accelerated and expanded qualification pathways to increase the supply of qualified health professionals. This includes accelerating the qualification of foreign-trained professionals and creating career advancement opportunities. This commitment is aligned with urgent recommendations from the Long-Term Care COVID‑19 Commission, which issued a report on October 23, 2020.
Investing in Personal Support Workers
Personal support workers (PSWs) play an integral role in the delivery of health care and social services. They provide a wide range of personal support services, such as bathing and general caregiving in hospitals, homes and community care and in long-term care. In the social services sector, these workers support individuals of all ages in residential settings and day programs.
The first wave of the pandemic exacerbated existing staffing challenges in both the health and social services sector, including shortages of PSWs. These important workers were supported with pandemic pay during the first wave of COVID‑19.
The government will continue to stand behind PSWs and direct support workers on the front lines of protecting the most vulnerable by providing $461 million in temporary wage increases for over 147,000 workers who deliver publicly funded personal support services. This investment will help the province attract and retain the workforce needed to care for patients, clients and residents in response to the COVID‑19 pandemic.
The Province is providing a temporary wage increase effective October 1, 2020 to over 147,000 workers who deliver publicly funded personal support services:
- $3 per hour for approximately 38,000 eligible workers in home and community care;
- $3 per hour for approximately 50,000 eligible workers in long-term care;
- $2 per hour for approximately 12,300 eligible workers in public hospitals; and
- $3 per hour for approximately 47,000 eligible workers in the children’s and social services sector to ensure that vulnerable individuals continue to receive personal care and supports for daily living from direct support workers.
The temporary wage enhancement will be reviewed on a regular basis and could extend through March 31, 2021, in connection with regulations made under the Reopening Ontario (A Flexible Response to COVID‑19) Act, 2020.
Accelerating Bed Development and Increasing Sector Capacity
Having a long-term care bed available, when it is needed, is a key component in Ontario’s strategy to make the health care system more efficient. With more than 38,000 people waiting to get into a long-term care home, relief is needed for those waiting to access a long-term care home and for long-term care operators who are facing significant barriers to building much needed beds. As a result, the government is accelerating the development of new and upgraded beds across Ontario.
Accelerating the Development of New and Upgraded Beds
The government remains committed to investing $1.75 billion to increase long-term care capacity and access for residents by building 30,000 long-term care beds, which will include air conditioning for any new and redeveloped homes.
To accelerate the construction of urgently needed long-term care projects, the Province has introduced a modernized funding model that will ensure timely bed availability that is responsive to the needs of the people of Ontario. The new funding model will help speed up construction by making needed changes to the Construction Funding Subsidy (CFS) and introducing a new upfront capital investment (see Table 1.1) recognizing the unique regional challenges faced by long-term care operators across the province.
| Market Segment | Incremental Increase to CFS1 | Per Cent of Upfront Capital |
|---|---|---|
| Large urban | $5.75 | 17% |
| Urban | $2.50 | 17% |
| Mid-sized | $2.50 | 10% |
| Rural | $2.75 | 12% |
Table 1.1 footnotes:
[1] Numbers listed above are incremental increases to the Construction Funding Subsidy (CFS) base of $18.03 per bed per day, and before any adjustments for home size and the ratio of basic to preferred accommodations. The development grant ranges from 10 per cent to 17 per cent of total eligible project costs, based on the market segment of where the project is constructed, up to the applicable maximum grant amount.
Source: Ontario Ministry of Long-Term Care.
Fast-Tracking the Building of New Long-Term Care Homes
On July 21, 2020, the government announced a new and innovative Accelerated Build Pilot Program that will enable the accelerated construction of four new long-term care homes in the Greater Toronto Area (GTA). This pilot is part of Ontario’s plan to create bed capacity faster than the traditional timeline for long-term care development. Partnering with Trillium Health Partners, Lakeridge Health and Humber River Hospital, in Mississauga, Ajax and Toronto, respectively, the pilot program will create new long-term care beds, which include features such as air conditioning and private or semi-private rooms. These innovative projects will leverage the use of hospital lands and a range of accelerating measures, such as modular construction and rapid procurement, to add up to 1,280 beds to the sector, with a targeted completion of early 2022.
Piloting Community Paramedicine for Long-Term Care
The Province is collaborating with health system partners to provide innovative resident-centred care to support those on the long-term care waitlist. Individuals who need long-term care services report they prefer to remain in their own homes for as long as possible. The government is listening by launching a Community Paramedicine for Long-Term Care program to help seniors remain stable in their own homes while also providing peace-of-mind for caregivers. This new program will provide individuals eligible for long-term care with 24/7 access to non-emergency support, through home visits and remote monitoring. The program will also leverage a model of community-based health care that allows paramedics to use their training and expertise to help seniors and their caregivers feel safe and supported in their own communities and potentially delay the need for a traditional long-term care bed.
The program will be immediately piloted in Renfrew County, York Region, the City of Ottawa, Cochrane District and Brant County while provincewide implementation continues to be explored.
Committing to Continuous Improvement
The Ontario government is committed to ensuring the long-term care system is safe, responsive and is delivering on the high-quality care that Ontario’s most vulnerable residents deserve by following expert advice and recommendations.
The Province is supporting safe and quality care across all long-term care homes by addressing recommendations made in the Public Inquiry into the Safety and Security of Residents in the Long-Term Care Homes System report. To date, more than 80 per cent of the recommendations are complete or underway.
Supporting People Suffering from Mental Health and Addictions Challenges
COVID‑19 has had significant impact on mental health and addictions (MHA) across the province. There has also been a disproportionate impact on individuals with existing mental health and addictions challenges. During the first wave of the COVID‑19 outbreak, the government invested $26.75 million to support a range of virtual and local MHA supports.
The government is also providing the people of Ontario with additional MHA services including:
- Additional community supports in both English and French, with a focus on stabilizing and enhancing mental health and addictions service delivery, and mobile crisis teams and safe beds for those experiencing a mental health crisis;
- More core children and youth mental health services, including walk-in clinics, counseling and therapy, day treatment and live-in treatment supports, focused on helping children in school, keeping children out of child welfare and supporting those in need of intensive services;
- A range of provincially available virtual supports including internet-based cognitive behavioural therapy, virtual addiction services, Kids Help Phone and continuation of supports for frontline COVID‑19 health care workers;
- Additional Indigenous supports;
- More critical rent supplements to support emergency short-term rentals during the second wave of COVID‑19;
- Additional support for interprofessional primary care teams; and
- A range of supports to seniors, those with disabilities, first responders (e.g., fire, police and paramedics) and vulnerable populations.
Increasing Mental Health Funding for Postsecondary Students
The Province is investing $19.25 million into mental health supports for postsecondary students in 2020–21, an increase of $3.25 million over last year. This funding will help students by strengthening community partnerships and increasing the number of mental health workers and programs at colleges, universities and Indigenous Institutes.
Continuing the Commitment to a Strong Health Care System
While the current priority is responding to the COVID‑19 pandemic, the government is steadfast in its commitment to continue to build a strong health care sector that meets the needs of the people of Ontario now and in the future.
Investing in Ontario’s Hospitals
Even before COVID‑19, the hospital system faced challenges such as use of unconventional beds, growing volumes, surgical and diagnostic waitlists and the need for capital improvements. That is why the government is investing $594 million in 2020–21 to provide the hospital sector with additional funding to address longstanding operational challenges.
The funding focuses on four key areas:
- Stabilizing Funding: the government is annualizing the investment made in the 2019 Ontario Economic Outlook and Fiscal Review to help small and medium-sized and multi-site hospitals to:
- Serve the people in Ontario living in rural and remote communities; and
- Help stabilize and sustain core services and programs at these hospitals and reduce the need for patients to travel across the province, country or border to receive care.
- Increasing Hospital Capacity: additional funding will be provided to support hospitals with newly opened beds and facility expansions, including the Centre for Addiction and Mental Health (CAMH), Brockville General Hospital, South Bruce Grey Health Centre – Kincardine Site and Cambridge Memorial Hospital. Hospital capacity will be increased by investing in equipment, maintenance, utilities, facility costs and hiring new staff.
- The government is also supporting innovative models of care such as Reactivation Care Centres, including in North York General Hospital, St. Joseph’s Hamilton, Southlake Regional Health Centre and Health Sciences North. These centres will help patients gain access to specialized care in the most appropriate setting, ensuring hospital beds are available for those who need them.
- Addressing Increasing Need: additional investments to help hospitals across Ontario address key challenges, such as a growing population, increasing access to highly specialized and innovative treatments, and reducing the use of unconventional beds. Funding will also provide hospitals with stability as the health sector undergoes transformation. New funding will:
- Provide additional across-the-board increases for all public hospitals, including small, medium, large community, teaching, specialty psychiatric and specialty children’s hospitals.
- Managing Waitlists: funding to address increased demand for non-elective and elective treatments and procedures including cardiac, neuroservices and cancer care. Funding will help:
- Maintain a high-quality health system and signal to stakeholders — including doctors, nurses and allied health professionals — that the province is a great place to practice; and
- Address wait times by adding up to 17,000 new MRI operating hours.
Building Infrastructure Capacity in Ontario Hospitals
Ontario is delivering on its commitment to address longstanding challenges in the hospital sector and respond to the COVID‑19 outbreak by building a connected and sustainable health care system centred on the needs of patients. The government is creating much-needed capacity at a critical time by investing more than $18 billion in capital grants over 10 years to build new and expanded hospital infrastructure and address urgent upgrades, including repairs and maintenance to help modernize hospitals across the province.
Through the Health Infrastructure Renewal Fund, the government is investing $175 million this year to support 129 hospitals across the province. This investment prioritizes urgent upgrades, repairs and maintenance projects, such as replacing roofs and windows, fire alarms and backup generators. Approximately $50 million of this funding will focus on supporting hospitals in their ongoing facility maintenance including updating HVAC systems, as well as enhancing other infection prevention and control measures.
In addition, there are almost 70 major hospital projects across the province that are currently under construction or progressing through various stages of planning. These investments are part of the government’s long-term plan to increase access to reliable, quality care so that patients and families receive excellent care when and where they need it.
Protecting Workplaces
Prioritizing workplace health and safety is important at any time, but even more so during the COVID‑19 pandemic. Employers face the challenge of creating an environment that prevents the spread of COVID‑19 and protects the health and safety of workers, supervisors and customers. Successfully overcoming this challenge will maintain business and consumer confidence and support economic recovery.
Hiring More Occupational Health and Safety Inspectors
The Province is hiring 98 new occupational health and safety inspectors to help ensure workplaces across Ontario are doing their part to prevent the spread of COVID‑19. With these new hires, Ontario will have more active inspectors than at any time in its history.
Providing COVID‑19 Workplace Safety Guidelines
To help employers develop safeguards that protect workers from COVID‑19, the Ministry of Labour, Training and Skills Development (MLTSD) has published COVID‑19 guidance resources for the workplace. The resources include sector-specific safety guidelines, videos, posters and a safety plan template that employers can adapt when creating COVID‑19 measures that suit their circumstances.
Renewing the Provincial Occupational Health and Safety Strategy
The government is renewing Ontario’s occupational health and safety strategy for 2021 to 2026, to ensure that workplaces practice health and safety in their everyday work. The strategy will use the best evidence available to improve training, knowledge and practices, help workers and employers meet their responsibilities and make safety easier to achieve for small businesses. A key part of the strategy will be preventing workplace fatalities, injuries and illnesses including infectious diseases such as COVID‑19.
Enhancing Infection Prevention and Control Capacity in the Social Services Sector
As Ontario continues to battle COVID‑19, the government is investing $30 million over two years to help service providers in the social services sector continue infection prevention and control (IPAC) measures. This includes supports to group homes, violence against women shelters, children’s aid societies and other congregate care settings.
The investment will help ensure service delivery partners have sufficient supports and resources in place to help reduce the number and severity of COVID‑19 outbreaks, resulting in better health outcomes for vulnerable populations. This includes resources at a community level to enhance knowledge and expertise regarding IPAC practices and assist with costs incurred by partners to meet IPAC protocols.
Building an Emergency Volunteer Unit
Throughout the COVID‑19 pandemic, the Ontario Spirit has shined bright as people across the province have stepped up to help their friends, family and fellow neighbours. Whether it was donating supplies, retooling their operations or supporting frontline staff, the people of Ontario took immediate action and responded to the crisis with compassion and generosity.
To support these efforts in the next emergency, the government intends to develop a new organization to oversee a Provincial Emergency Volunteer Unit. This organization will develop and oversee a pool of volunteers who pre-register to help during an emergency. It will be tasked with recruiting volunteers from diverse backgrounds, including age, geography and skillset. The organization will primarily focus on large-scale emergencies such as natural disasters or health crises but will be tasked with investigating how it can support the broader volunteer sector and sustain the culture of volunteerism demonstrated by the Ontario Spirit this year.
The government will consult with the volunteer sector this winter and outline a plan to launch this organization in the spring Budget.
Chart Descriptions
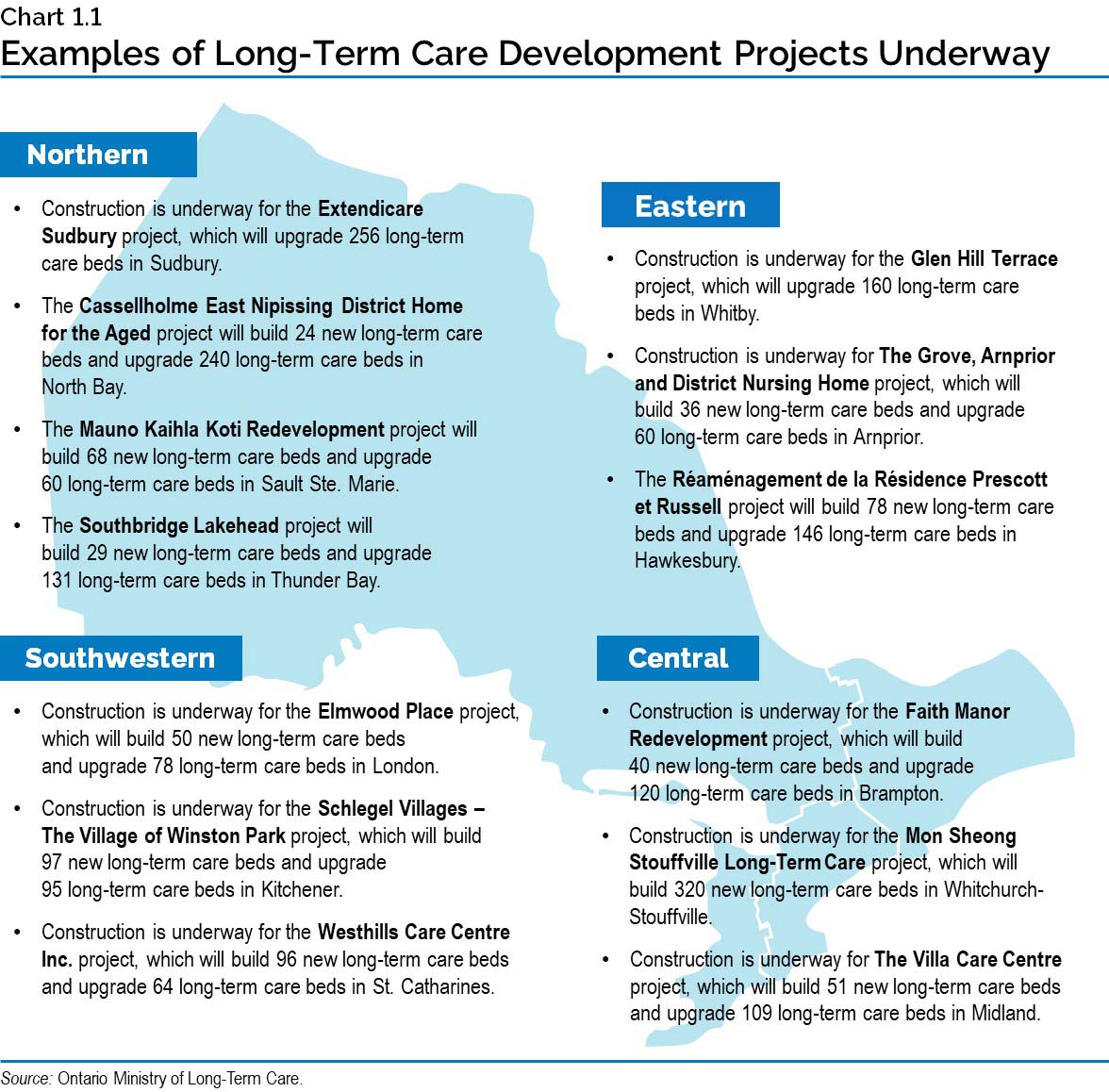
Chart 1.1: Examples of Long-Term Care Development Projects Underway
This map provides examples of long-term care development projects underway across Ontario.
Northern: Construction is underway for the Extendicare Sudbury project, which will upgrade 256 long-term care beds in Sudbury The Cassellholme East Nipissing District Home for the Aged project will build 24 new long-term care beds and upgrade 240 long-term care beds in North Bay; The Mauno Kaihla Koti Redevelopment project will build 68 new long-term care beds and upgrade 60 long-term care beds in Sault Ste. Marie; The Southbridge Lakehead project will build 29 new long-term care beds and upgrade 131 long-term care beds in Thunder Bay.
Eastern: Construction is underway for the Glen Hill Terrace project, which will build upgrade 160 long-term care beds in Whitby; Construction is underway for the The Grove, Arnprior and District Nursing Home project, which will build 36 new long-term care beds and upgrade 60 long-term care beds in Arnprior; The Réaménagement de la Résidence Prescott et Russell project will build 78 new long-term care beds and upgrade 146 long-term care beds in Hawkesbury.
Central: Construction is underway for the Faith Manor Redevelopment project, which will build 40 new long-term care beds and upgrade 120 long-term care beds in Brampton; Construction is underway for the Mon Sheong Stouffville Long-Term Care project, which will build 320 new long-term care beds in Whitchurch-Stouffville; Construction is underway for The Villa Care Centre project, which will build 51 new long-term care beds and upgrade 109 long-term care beds in Midland.
Southwestern: Construction is underway for the Elmwood Place project, which will build 50 new long–term care beds and upgrade 78 long-term care beds in London; Construction is underway for the Schlegel Villages - The Village of Winston Park project, which will build 97 new long-term care beds and upgrade 95 long-term care beds in Kitchener; Construction is underway for the Westhills Care Centre Inc project, which will build 96 new long-term care beds and upgrade 64 long-term care beds in St. Catharines.
Source: Ontario Ministry of Long-Term Care
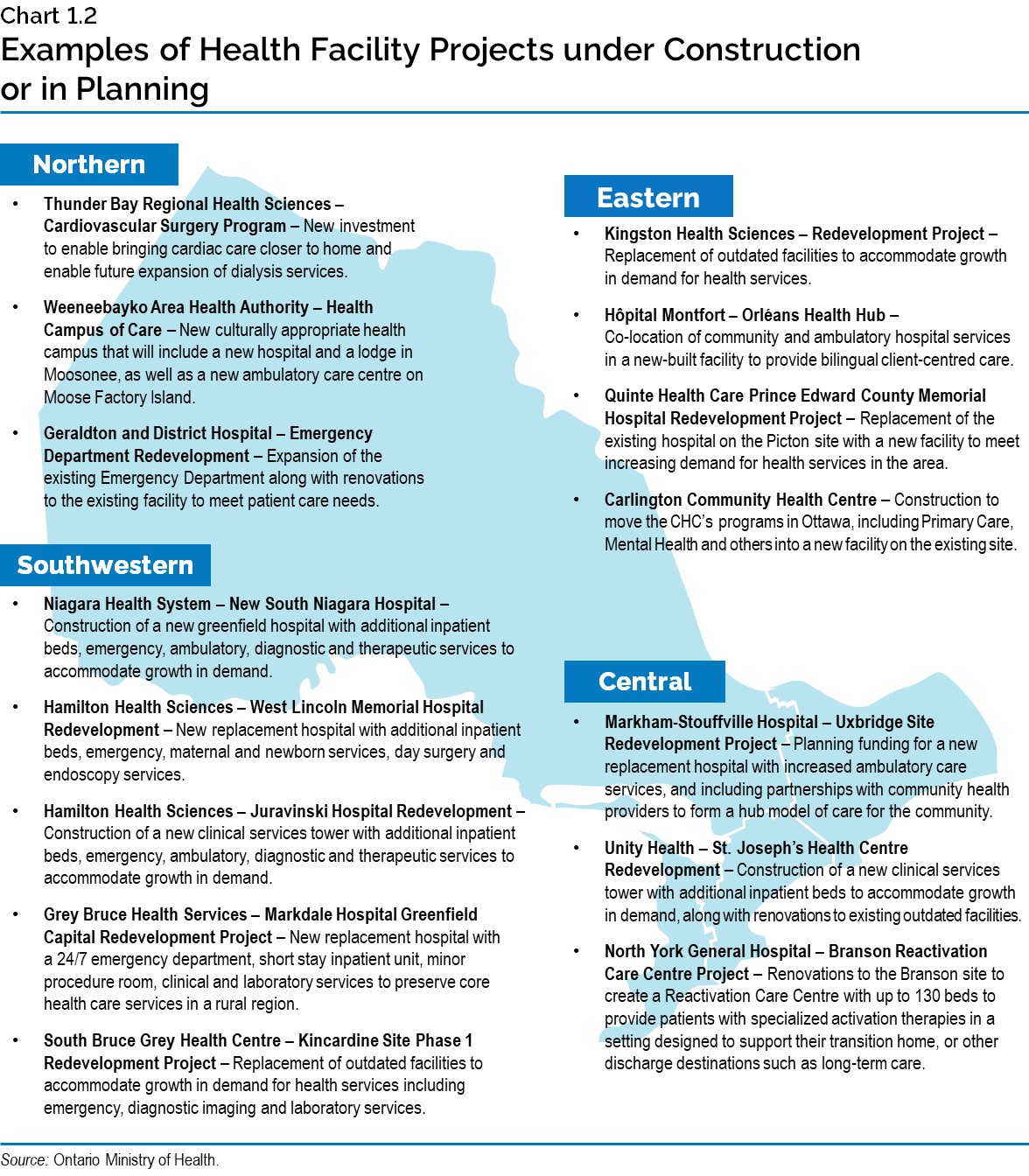
Chart 1.2: Examples of Health Facility Projects under Construction or in Planning
This map provides examples of health facility projects under construction or in planning across Ontario.
Northern: Thunder Bay Regional Health Sciences – Cardiovascular Surgery Program – New investment to enable bringing cardiac care closer to home and enable future expansion of dialysis services. Waypoint Hospital / Chigamik CHC – Mental Health and Community Co-Location – Co-location of hospital ambulatory mental health services with the Chigamik Community Health Centre. Weeneebayko Area Health Authority – Health Campus of Care – New culturally appropriate health campus that will include a new hospital and a lodge in Moosonee, as well as a new ambulatory care centre on Moose Factory Island. Geraldton District Hospital – Emergency Department Redevelopment – Expansion of the emergency department along with renovations to the existing facility to meet patient care needs.
Eastern: Kingston Health Sciences – Redevelopment – replace outdated facilities and accommodate growth in demand for health services. Hôpital Montfort – Orléans Health Hub - Co-location of community and ambulatory hospital services in a new-built facility to provide bilingual client-centered care. Quinte Health Care Prince Edward County Memorial Hospital Redevelopment Project – Replacement of the existing Hospital on the Picton site with a new facility to meet increasing demand for health services in the area. Carlington Community Health Centre – Construction to move the CHC’s programs in Ottawa, including Primary Care, Mental Health and others into a new facility on the existing site.
Central: Markham-Stouffville Hospital – Uxbridge Site Redevelopment Project – Planning funding for a new replacement hospital with increase ambulatory care services and including partnerships with community health providers to form a hub model of care for the community. Unity Health – St. Joseph’s Redevelopment – Construction of a new clinical services tower with additional inpatient beds to accommodate growth in demand, along with renovations to existing outdated facilities. North York General Hospital – Branson Reactivation Care Centre Project – Renovations to the Branson site to create a Reactivation Care Centre with up to 130 beds to provide patients with specialized activation therapies in a setting designed to support their transition home, or other discharge destinations such as long-term care.
Southwestern: Niagara Health System – New South Niagara Hospital - Construction of a new greenfield hospital with additional inpatient beds, emergency, ambulatory, diagnostic and therapeutic services to accommodate growth in demand. Hamilton Health Sciences – West Lincoln Memorial Hospital Redevelopment – New replacement hospital with additional inpatient beds, emergency, maternal and newborn services, day surgery and endoscopy services. Hamilton Health Sciences – Juravinski Hospital Redevelopment – Construction of a new clinical services tower with additional inpatient beds, emergence, ambulatory, diagnostic and therapeutic services to accommodate growth in demand. Grey Bruce Health Services – Markdale Hospital Greenfield Capital Redevelopment Project - New replacement hospital with a 24/7 emergency department, short stay inpatient unit, minor procedure room, clinical and laboratory services to preserve core health care services in a rural region. South Bruce Grey Health Centre – Kincardine Site Phase 1 Redevelopment Project – Replacement of outdated facilities to accommodate growth in demand for health services including emergency, diagnostic imaging and laboratory services.
Chart 1.3: Canada Health Transfer National Entitlement: A Fair Federal Share vs. the Status Quo
This chart illustrates the gap between a fair federal share (35 per cent) and status quo (22 per cent) in Canada Health Transfers. In 2021–22, this gap represented $28 billion nationally, and over $10 billion for Ontario. By 2040, this gap is estimated to grow to roughly $100 billion nationally, and $40 billion for Ontario, as the CHT is projected to decline further to 16 per cent of provincial–territorial health spending.
Sources: Council of the Federation (September 18 Communiqué) estimate of provincial–territorial health costs; and Ontario Ministry of Finance calculations.