Introduction
COVID‑19 has impacted every aspect of Ontario’s economy and communities, but the virus has first and foremost caused a global health tragedy.
This is why Ontario’s primary focus since March 2020 has been protecting people’s health and well‑being. Premier Ford made a simple, non-negotiable promise to the people of Ontario — this government will do whatever it takes to keep the people of Ontario safe.
The government has made good on this promise starting with the actions taken in March 2020 with Ontario’s Action Plan: Responding to COVID‑19, followed by the 2020 Budget introduced on November 5, 2020, and now, with Ontario’s Action Plan: Protecting People’s Health and Our Economy.
From the very beginning, Ontario has focused on ensuring that hospitals and the health care system more broadly have the health care workers and the space needed to care for anyone who becomes ill. The government recently announced an additional $125 million to fund over 500 critical care and high intensity hospital beds in areas with high rates of transmission. Ontario will invest an additional $1.8 billion in the hospital sector in 2021–22 bringing the total additional investment in hospitals since the start of the pandemic to over $5.1 billion. This is providing for more than 3,100 beds to increase capacity and reduce occupancy pressures caused by COVID‑19. The creation of over 3,100 new beds is the equivalent of six new large community hospitals in the province — this is an historic investment.
Ensuring COVID‑19 patients are cared for is a fundamental responsibility for the government but preventing and controlling the spread of the virus is the ultimate goal. This is why Ontario has made available over $1.4 billion to access personal protective equipment (PPE), enabling the province to purchase more than 315 million masks and more than 1.2 billion gloves, while also working with the private sector to increase domestic production capacity of PPE in Ontario. This is also why over $100 million has been invested in dedicated infection prevention and control in hospitals, long-term care and other settings.
As COVID‑19 vaccines are being rolled out, the use of a comprehensive testing strategy is an important tool in identifying and slowing the spread of COVID‑19. Ontario is building on its testing strategy by investing $2.3 billion in 2021–22 and is expanding the use of rapid testing in high priority areas, such as schools, congregate settings, workplaces and high priority communities.
Over the past year, COVID‑19 vaccines have been viewed as the light at the end of the tunnel. They have provided a beacon of hope that the people of Ontario will someday embrace loved ones in a warm hug, enjoy a cup of coffee with a friend, and once again see colleagues in person. Nothing is more important to the government than distributing vaccines as quickly and efficiently as possible. This is why, beginning in 2020–21, Ontario is investing more than $1 billion as part of Ontario’s vaccination plan, including $50 million to support vaccinations in First Nations and urban Indigenous communities.
Since the early days of the pandemic, it has become clear that COVID‑19 does not pose the same risk to everyone equally. Seniors are especially vulnerable, and COVID‑19 has had a particularly tragic impact on those living in long-term care homes as well as their families, including here in Ontario. This is why Ontario is investing up to $650 million in additional funding in 2021–22 to protect loved ones in long-term care from the virus and to stabilize homes, in addition to providing $30 million annually to recruit, retain and train infection prevention and control staff in long-term care homes across the province.
This is also why the government has renewed its commitment to fix long-standing challenges in the long-term care sector, including building and updating long-term care homes. In addition to the government’s original investment of $1.75 billion, Ontario is investing another $933 million over the next four years to build more long-term care beds. These combined investments will support Ontario’s commitment to build 30,000 long-term care beds. In contrast, between 2011 and 2018, there were only 611 long-term care beds built across the province. In addition to traditional long‑term care development, Ontario is also building four new long-term care homes faster through the innovative Accelerated Build Pilot Program.
The province is also initiating the largest recruitment and training of personal support workers (PSWs) in Ontario history, to reduce unreasonably long waitlists and provide better care for residents. Ontario is the first province to commit to a new standard of quality care for residents. Ontario’s Action Plan: Protecting People’s Health and Our Economy confirms this commitment and provides $4.9 billion over four years to make this ambitious vision a reality. And the province is acting now with the accelerated training of almost 9,000 PSWs.
While COVID‑19 has caused much pain, suffering and fear, Ontario is already seeing a significant positive impact from vaccinations across the province. The people of Ontario can be confident that their government will continue to protect them now, and when the pandemic is finally brought under control.
Ontario’s Action Plan: Protecting People’s Health and Our Economy brings the government’s total investment to protect people’s health to $16.3 billion.
Defeating COVID‑19
The people of Ontario look forward to the day when the COVID‑19 pandemic is in the past — when people no longer fear for their health, and when the current public health restrictions to slow the spread can finally be lifted. Since day one, Ontario has focused on fighting the virus so life can get back to normal. Ontario’s Action Plan: Protecting People’s Health and Our Economy builds on the government’s strong record of investments to beat COVID‑19 once and for all.
Vaccinating Ontario

The key to defeating COVID‑19 is ensuring every person who wants a vaccine gets a vaccine. Working with partners — including the federal government and local public health units — to vaccinate the people of Ontario is the government’s most urgent priority. Nothing is more important. This is why the government is investing more than $1 billion as part of Ontario’s vaccination plan, beginning in 2020–21 to support the administration, distribution and rollout of Ontario’s COVID‑19 vaccination campaign, including $50 million to support vaccinations in First Nations and urban Indigenous communities.
Ontario’s vaccination plan is led by the government’s COVID‑19 Vaccine Distribution Task Force chaired by General (retired) Rick Hillier, former Chief of Defence Staff for the Canadian Armed Forces. The rollout of the vaccines is based on the government’s Ethical Framework for COVID‑19 Vaccine Distribution and is founded on the following principles:
- Minimize Harms and Maximize Benefits: to reduce overall illness and death related to COVID‑19; protect those at greatest risk of serious illness and occupational factors; protect critical infrastructure and promote social and economic well-being;
- Equity: to distribute COVID‑19 vaccines without bias or discrimination, and to ensure high-risk groups and those most greatly impacted by the COVID‑19 pandemic have access to the vaccine;
- Fairness: to ensure that every individual, within the same priority group, has the same opportunity to be vaccinated, using an inclusive, consistent process that is tailored to the unique needs of Ontario’s many and varied communities;
- Transparency: to ensure the principles, rationale, decision-making processes and plans for COVID‑19 prioritization are clear, understandable and effectively communicated to the public;
- Legitimacy: to ensure decisions are based on the best available scientific evidence, shared values and input from affected parties, including those historically underrepresented so that the resulting decisions have the intended impact; and
- Public Trust: to ensure decisions and decision-making processes are informed by these principles to advance public confidence and trust in Ontario’s COVID‑19 vaccination program.
Ontario has a comprehensive and integrated vaccination plan that starts with the most vulnerable people of Ontario and frontline health care workers. Phase One of Ontario’s vaccination rollout is well underway, and as of early March 2021, over 80 per cent of the long-term care residents are fully immunized and public health units are working with homes to vaccinate staff and essential caregivers as a priority. The government has enabled and is mobilizing additional health care providers including registered nurses, nurse practitioners, registered practical nurses, pharmacists, pharmacy technicians, paramedics and pharmacy students to administer the vaccine. This is the Team Ontario approach.
The plan aims to reduce virus transmission and infection, as well as hospitalizations. As the supply of vaccines increases, the people of Ontario will be able to get vaccinated in several new settings. In addition to hospitals, mobile clinics and mass vaccination clinics, the province is working with the pharmacy sector and with primary care professionals to offer vaccinations in primary care settings and community locations in collaboration with public health units.
Ontario’s vaccination rollout will culminate with Phase Three when vaccines are available for everyone who wishes to be immunized.
| Phase 1 | Phase 2 | Phase 3 |
|---|---|---|
| High-risk populations (approximately 1.8 million) December 2020 – March 2021
|
Mass deliveries of vaccines (approximately 9 million) April 2021 – July 2021
|
Steady state July 2021 Onwards
|
| Distribution through: hospital site clinics, mobile teams, site‑specific clinics, mass vaccination clinics (late March) |
Distribution through: mass vaccination clinics, pharmacies, primary care, site-specific clinics, mobile teams, mobile sites, public health units |
Distribution through: mass vaccination clinics, pharmacies, primary care, site-specific clinics, mobile teams, mobile sites, public health units |
Table 1.1 footnotes:
Note: Timelines are estimates and may change dependent on vaccine supply.
Source: Ontario Ministry of Health.
The government’s top priority is to ensure that it has the plan, the processes and the people in place to administer vaccines as quickly as possible while also preparing to receive shipments as they arrive. The plan activates the entire health care infrastructure, including public health units, hospital clinics, mass vaccination sites, mobile clinics, pharmacies and primary care. On the ground, the plan is adapting to the unique situation of each of the province’s 34 public health units, reflecting the diverse populations and vast geography of the province — all with the aim of vaccinating the people of Ontario as soon as possible.
Helping the Vulnerable Get Vaccinated
A lack of mobility or transportation should not prevent anyone from getting vaccinated. Ontario is investing $3.7 million in 2021–22 to help remove barriers and provide safe, accessible transportation for persons with disabilities and older adults with limited mobility to travel to their COVID‑19 vaccination appointments.
This will help remove accessibility and financial barriers that may prevent these individuals from travelling to vaccination appointments.
Ensuring Indigenous Communities Have Access to Vaccines
Indigenous communities are at higher risk for COVID‑19 outbreaks and have challenges in accessing health care, which can lead to more severe outcomes. Available health data also indicates that Indigenous peoples generally have higher rates of chronic diseases that may put them at greater risk of health complications if exposed to COVID‑19.
Ontario is investing $50 million to support community-led vaccination efforts in First Nations and urban Indigenous communities. This investment will provide additional health care supports, including more public health capacity and greater access to testing in Indigenous communities. This funding will also help to set up onsite clinics to support vaccine roll-out, working with Indigenous communities.
Operation Remote Immunity, led by Ornge, is vaccinating adults in the 31 fly-in First Nation communities and Moosonee in Northern Ontario. As of the first week of March, all adults in these communities have been offered their first dose of the COVID‑19 vaccine and second doses have commenced for some communities. Planning for vaccine distribution to additional First Nation communities and to urban Indigenous populations is underway.
Increasing Access to COVID‑19 Testing
While vaccines are the key to ending the pandemic, stopping the spread of the virus in the meantime remains vital to protect lives. Ontario is investing over $3.7 billion over two years, including $2.3 billion in 2021–22, in a comprehensive testing strategy. The ongoing effort will ensure timely access to testing — targeting testing to vulnerable communities, as well as expanding the capacity to process COVID‑19 tests effectively.
Timely, high-quality COVID‑19 testing is a critical component to respond to the virus. Ontario has expanded all aspects of testing ranging from COVID‑19 specimen collection, transportation, laboratory analysis and reporting.
Ontario continues to ramp up efforts in testing, tracing and isolating cases of COVID‑19. The people of Ontario can receive COVID‑19 tests at one of over 500 testing sites located at assessment centres, participating community laboratories, or participating pharmacies across the province. The government has deployed rapid testing to provide faster results in regions of high transmission and in rural and remote areas.
Laboratory-based polymerase chain reaction (PCR) testing remains the gold standard in diagnostic tests and the province has the capacity to perform 105,000 tests per day. Additionally, over 90 per cent of individuals who have been tested receive test results within two days. As of March 1, 2021, over 11 million tests have been completed.
Ontario is leading Canada in the number of rapid tests deployed, leveraging the full spectrum of testing tools and has deployed over 3.1 million rapid tests to high priority settings as of late February 2021. As of March 8, 2021:
- More than 1.8 million rapid antigen tests have been deployed to 567 long-term care homes. Going forward, the province will provide approximately 385,000 tests per week for asymptomatic staff, support workers, essential caregivers, students and volunteers;
- Approximately 323,000 rapid antigen tests have been deployed to 202 retirement homes. Going forward, the province plans to provide up to 118,000 tests per week for asymptomatic staff and essential visitors such as personal support workers or other care providers entering retirement homes;
- 232,000 rapid tests have been sent to 39 essential industry sites. The province will continue to deploy rapid testing in workplaces, including up to 300,000 COVID‑19 tests per week for asymptomatic staff in key sectors such as manufacturing, warehousing, supply chain, mining, construction and food processing; and
- Ontario is also working with a broad range of congregate care settings to onboard interested organizations to deploy rapid antigen tests in the coming weeks, including to residential mental health centres, adult and children’s residences, supportive housing and other congregate living settings.
Going forward, the province will be able to deploy up to approximately one million tests per week across targeted sectors.
Ontario continues to ensure that anyone who needs a test can get a test, and to have results as quickly as possible.
Ensuring Ontario Always has Enough PPE

While most people had never heard the term PPE before last March, personal protective equipment has become a part of everyday life. It protects Ontario’s vulnerable loved ones, keeps frontline heroes safe and is essential to keeping the economy and communities functioning during the COVID‑19 pandemic. Ontario has purchased more than 315 million masks and more than 1.2 billion gloves since the beginning of COVID‑19, many from manufacturers and suppliers right here at home. Ontario has also made a commitment to ensure the province is never again at the mercy of another jurisdiction for PPE.
On November 5, 2020, Ontario established Supply Ontario, a new provincial agency to operate as a modern and efficient single supply chain organization for the Ontario Public Service and the broader public sector, including the health sector. Supply Ontario will build on the efforts of this government to continue to ensure that the province has a strong supply chain for PPE and other essential supplies and equipment required to protect the people of Ontario. It will leverage the buying power of the province, while taking advantage of the innovation and creativity of local businesses.
In the fight against COVID‑19, Supply Ontario will help ensure that schools, hospitals and the entire public sector have the critical supplies and equipment needed to keep individuals and families safe. Building on previous investments, Ontario is continuing to procure surgical and procedural masks and N95 respirators, gloves, gowns and face shields. To date, Ontario has made $1.4 billion available for PPE.
Creating More COVID‑19 Hospital Capacity
When Ontario families face a health challenge, they need to be confident they can get the care and treatment they require at any hospital in the province. While hospitals faced many challenges even before the pandemic, COVID‑19 has stretched them to the limit. This is why Ontario is making the necessary investments to ensure hospitals will be able to care for people if and when it is required. In fact, the government has added more than 3,100 new beds, the equivalent of six large community hospitals, to the health care system since the beginning of COVID‑19.
Ontario will invest an additional $1.8 billion in the hospital sector in 2021–22 bringing the total additional investment in hospitals since the start of the pandemic to over $5.1 billion. Building on the $3.4 billion provided in 2020–21, this additional $1.8 billion investment in 2021–22 includes:
- $760 million to support more than 3,100 hospital beds to help the sector continue to provide care for COVID‑19 patients as well as other patients;
- $300 million to reduce surgical backlogs from delayed or cancelled surgeries and procedures due to the COVID‑19 pandemic; and
- $778 million to support hospitals to keep pace with patient needs and to increase access to high‑quality care.
Clearing the Surgical and Procedural Backlog Caused by COVID‑19
As Ontario’s three-phase distribution plan for vaccinations is underway to protect the people of Ontario from COVID‑19, the government is working closely with hospitals to help them return to normal operations. This will allow the hospital sector to recover, address the surgical backlog and improve access to care.
Ontario is investing over $610 million, including $300 million in 2021–22 to address the surgical backlog from delayed or cancelled surgeries and procedures due to the COVID‑19 pandemic. Funding will help hospitals keep operating rooms open late in the evening to complete up to 52,000 surgical hours of elective surgeries and will address the MRI/CT backlog. This investment will also be used to create a centralized provincial surgical waitlist program to help reduce delays in scheduling and help match patients to surgeons with shorter wait times.
Protecting Communities Most Affected by COVID‑19
COVID‑19 has disproportionately impacted racially diverse, newcomer and low-income communities. This is why Ontario is investing $50 million in additional support to protect these communities.
Restrictions, such as stay-at-home orders and self‑isolation, may be insufficient to contain the spread of COVID‑19 due to circumstances beyond the control of the residents in these communities. The additional funding will include support for targeted and tailored community outreach and education using Community Ambassadors, mobile testing sites and distribution of PPE kits. This funding will also provide case management support that connects individuals to critical services, including access to isolation centres to help individuals safely self-isolate and reduce COVID‑19 transmission.
The ability to isolate safely is essential to help stop the spread of COVID‑19 in our community. We were pleased about the arrival of new isolation centres in Brampton. More isolation centres right in our neighbourhoods means Brampton residents can ensure family at home stay safe.
Mayor Patrick Brown
City of Brampton
This additional support builds upon the previous investments provided under the High Priority Communities Strategy, including $12.5 million to help fund lead community agencies and community partners in 15 priority neighbourhoods in Durham, Peel, Toronto, York and Ottawa, as well as $42 million for COVID‑19 isolation centres. This funding helps keep people and communities safe, by helping people in some of the hardest hit neighbourhoods self-isolate and by supporting additional community outreach and education on COVID‑19 safety measures. This investment will also deliver enhanced interventions to stop the spread of COVID‑19, such as mobile testing, and promote vaccine uptake in these vulnerable communities, home to individuals who often work in higher risk essential sectors. Funding also provides emergency income supports to vulnerable populations in identified priority communities.
Providing COVID‑19 Supports for Indigenous Peoples and Communities
The second wave of the COVID‑19 pandemic has presented unique challenges for Indigenous communities and organizations. There is an urgent need to support First Nations, Métis and Inuit populations, including Indigenous elders, low-income workers, single-parent families and those experiencing homelessness.
Building on prior investments during the COVID‑19 pandemic, Ontario is investing an additional $4 million in 2021–22 to support First Nations, Métis and Inuit populations. This includes funding for contact tracing, self-isolation and resources to combat food insecurity and housing shortages. These resources will assist individuals and communities throughout the pandemic and during the recovery period, supporting well-being and financial stability. This is in addition to the $50 million made available to ensure First Nations and urban Indigenous communities can be vaccinated and brings Ontario’s total investment to protect Indigenous peoples to more than $120 million since the beginning of COVID‑19.
By continuing to provide COVID‑19 supports, Ontario is providing services that prevent crisis situations, while more vaccinations become available to priority populations including Indigenous peoples. Culturally responsive supports to First Nations, Métis and Inuit populations are a key part of Ontario’s plan to beat COVID‑19.
Ramping Up COVID‑19 Digital Rapid Response
In the past year, digital and data services helped the people of Ontario navigate these difficult times, by providing easy access to vital public health information and services in real time. In response to COVID‑19, the province took action to deliver benefits quickly to those who needed it most, including enhancing access to virtual care so more patients can see their doctor by phone or virtually. As a result, people have better access to more convenient online options and publicly available data to help them make important decisions for their lives.
Fixing Long-Term Care

Long-standing challenges in the long‑term care system were heightened by the COVID‑19 pandemic and have had tragic consequences for too many Ontario families. Rising complexity of care, staffing shortages, aging infrastructure and a long list of people waiting for beds are just some of the challenges in long-term care. While these challenges have been ignored by successive governments, fixing the long‑term care system is an urgent priority for this government.
Protecting Long-Term Care Residents from COVID‑19
COVID‑19 has had a particularly devastating impact in long-term care homes around the world, including in Ontario. This government is committed to protecting residents, caregivers and staff from future outbreaks by building on earlier investments and pandemic response measures.
As of winter 2021, the government has made record investments to protect long-term care since the start of the COVID‑19 pandemic. Ontario’s total additional funding to protect long-term care homes since the start of the COVID‑19 pandemic is $1.38 billion. This investment helped long-term care homes increase staffing and improve infection prevention and control practices. Building on this initial investment, Ontario is making an additional $650 million available in 2021–22 to continue to protect long-term care residents, bringing the government’s total additional investment to over $2 billion. As the rollout of COVID‑19 vaccines continues, this funding will help homes prevent the spread of the virus, increase staffing supports and purchase additional supplies and equipment.
We gratefully acknowledge the government for their continued supports for emergency pandemic funding to enhance safety in our homes by prioritizing testing, vaccinations, personal protective equipment and other essential supports.
Ruth McFarlane
CEO, Durham Christian Homes and
Vice Chair, Board, Ontario Long Term Care Association
Ontario is also continuing funding announced in the 2020 Fall Preparedness Plan for Health, Long‑Term Care and Education to retain newly hired infection prevention and control staff as well as train staff in infection prevention practices. This $30 million annual investment will help protect residents, staff and families today and into the future.
Ensuring Loved Ones Have Access to Care
Ontario is committed to creating a safe and modern long-term care system that provides the highest quality of care for loved ones when and where they need it. With an aging population and growing demand, the construction of more modern long-term care homes is necessary. This is why the government is accelerating the creation of new and upgraded beds across Ontario.
Building and Upgrading More Beds, Faster
In addition to the government’s original investment of $1.75 billion, Ontario is investing another $933 million over the next four years to build more long-term care beds. These combined investments will support Ontario’s commitment to build 30,000 long-term care beds. In contrast, between 2011 and 2018, there were only 611 long-term care beds built across the province.
To expedite long-term care development, the government is moving forward with the approval of 9,478 new beds and the upgrade of an additional 5,212 existing beds.
In selecting projects, Ontario is implementing lessons learned on improved infection prevention and control measures, particularly the elimination of three- and four-bed ward rooms. Long-term care development projects will also add capacity for high need areas, Francophone and Indigenous communities and promote the development of campuses of care. The government is also providing funding for air conditioning for homes.
These most recent allocations will result in a development pipeline of 20,161 new spaces — representing more than two thirds of the government’s commitment to build 30,000 new beds by 2028 — as well as 15,918 upgraded spaces.
Improving Quality of Life in Long-Term Care Homes
To ensure loved ones in long-term care homes are properly cared for, the government is making up to $246 million available over the next four years to prioritize upgrades that will enhance resident safety and comfort, such as air conditioning. This investment will help fund projects in the long-term care sector including important upgrades to ventilation and renovations that will improve infection prevention and control.
Providing the Best Long-Term Care in Canada
Ontario is taking monumental steps to protect the most vulnerable people in the province with plans to increase average daily direct care per resident to four hours — making Ontario the first in Canada to commit to this level of care. Over the next four years, the average hours of daily direct care will increase to four hours, from the current 2.75 hours. To support this plan, the government will invest up to $1.9 billion annually by 2024–25, or $4.9 billion over the next four years. In addition, this funding will support a 20 per cent increase in direct care time by allied health professionals including physiotherapists and social workers.
Delivering on a Provincial Staffing Plan for Long-Term Care
Working in Partnership to Deliver Quality Care
Ontario’s ambitious plan to ensure long-term care residents receive an average of four hours of daily direct care will require hiring and training tens of thousands of new staff over the next four years. This is why the government has launched the most ambitious recruitment and training program in Ontario’s history.
This training will help Ontario build a workforce that supports our most vulnerable at a time of growing need. It also means jobs, income and stability for thousands of workers who support their families and keep our economy running by shopping at local businesses. The benefits are exponential.
Eduardo Almeida
First Vice-President/Treasurer
Ontario Public Service Employees Union
Provincial investments will support ongoing hiring of additional staff, including registered nurses, registered practical nurses and personal support workers. Ontario is supporting continued professional development, to increase the supply of long-term care staff and to improve staff retention. The government is also working with long-term care employers to improve working conditions, for example through increased full-time employment, and innovative approaches to work and technology. Finally, Ontario is continuing to work with the sector to support effective and accountable leadership in long-term care homes.
Continuing Support for Workers Providing Personal Support Services
The government is extending the wage enhancement for over 147,000 workers who deliver personal support services. This wage enhancement will continue for eligible workers until June 30, 2021 and it will continue to be reviewed. The wage enhancement is part of a broad set of initiatives aimed at stabilizing staffing levels and supporting current and future frontline workers.
Expanding Personal Support Worker Training
Ontario is investing over $121 million to support the accelerated training of almost 9,000 personal support workers (PSWs), which is the largest recruitment of PSWs in Ontario’s history. This includes $115 million to train up to 8,200 new PSWs through publicly funded colleges. The accelerated PSW training program is a publicly funded, tuition-free opportunity for 6,000 new students and is expected to take six months to complete, rather than the typical eight months. This program will provide students with a combination of coursework and a three-month paid experiential learning opportunity at a long-term care home or in a home and community care environment. Additionally, nearly 2,200 existing students will be eligible to receive a $2,000 tuition grant to help them complete their studies, as well as a stipend to complete the clinical placement part of their training.
In February 2021, Ontario announced an investment of more than $4.1 million for eight training projects, including in regions hit hard by the COVID‑19 pandemic. This investment will support the training of 373 new PSWs and provide them with health and safety resources. In addition, the government provided up to $2.4 million through a pilot scholarship program to fund the training costs of up to 300 students for PSW positions in long-term care homes in the Ottawa area.
Scaling Up Health Human Resources
To alleviate staffing pressures and protect the vulnerable people of Ontario, the province is scaling up Health Human Resources Planning to ensure the long-term care sector and the health care system have the capacity to continue quality service delivery. This plan will ensure Ontario’s most vulnerable patients receive the care they need, when and where they need it. These efforts will also ensure that frontline workers have the support they need to provide care for the people of Ontario.
In addition, the province is providing financial support to Ryerson University in the planning for a proposal for a new institute of medical education in Brampton.
Hiring More Staff for Retirement Homes
Many retirement home residents depend on PSWs and nurses to provide them with the care they need. Starting in 2021–22, Ontario is investing $2 million over two years to attract new PSWs and nurses to work in retirement homes.
Through this initiative, PSWs will receive a financial grant of $5,000 for a six-month commitment to work in a retirement home. Nurses will receive $10,000 for a one-year commitment to work in a retirement home.
Expanding Community Paramedicine for Long-Term Care
Through the Community Paramedicine for Long-Term Care program, seniors can receive the quality care and service they need at home. While Ontario is accelerating the development of thousands of new long-term care beds to increase capacity, this innovative resident-centred program will allow seniors to live longer in the comfort of their own homes.
Ontario began a pilot in five communities in 2020 and is investing approximately $160 million over three years to support the program in 33 communities, see Table 1.2 for the details.
| Community Name |
|---|
| Chatham-Kent |
| Cornwall and Stormont, Dundas, Glengarry |
| Dufferin County |
| Essex County and Windsor |
| Frontenac County and Kingston |
| Greater Sudbury |
| Grey County |
| Guelph and Wellington County |
| Haliburton County |
| Halton Region |
| Hamilton |
| Hastings County, Belleville, Quinte West and Prince Edward County |
| Lambton County |
| Lanark County |
| Brant County |
| City of Ottawa |
| Cochrane District |
| Leeds-Grenville |
| Manitoulin and District of Sudbury |
| Middlesex County and London |
| Muskoka |
| Niagara Region |
| Nipissing District |
| Parry Sound |
| Peel Region |
| Rainy River District |
| Simcoe County |
| Thunder Bay and District |
| Toronto |
| Waterloo Region |
| Norfolk County |
| Renfrew County |
| York Region |
Table 1.2 footnotes:
Source: Ontario Ministry of Health.
Caring for People
Compassion is a defining value of the people of Ontario. This value is perhaps best illustrated by the care and professionalism of the thousands of frontline workers in Ontario’s health care system. COVID‑19 has highlighted the work of these health care heroes, whose efforts have been vitally important before the pandemic and will remain so after. This is why the government is making investments to ensure people who need care can access it, where and when it is required.
Making Record Investments in Hospitals

Even before COVID‑19, Ontario was working to ensure patients could access high-quality care at any hospital across the province when they needed it. And, as the province continues to combat COVID‑19, Ontario remains committed to supporting the province’s hospitals. This is why the government is investing an additional $5.1 billion in hospitals since the start of the pandemic, including investments in 2021–22 of $760 million to help hospitals continue to respond to COVID‑19, an additional $300 million to reduce surgical backlogs and $778 million to help hospitals keep pace with patient needs and to increase access to high-quality care. This brings total additional investment for hospitals to $1.8 billion in 2021–22.
The additional $778 million funding for patient needs will support four key areas:
- Caring for a Growing and Aging Population: new investments to provide patients additional surgical and diagnostic procedures, which include funding for cancer and chronic kidney disease services, cardiac services, neurological services, organ and tissue donation and transplantation, and MRI/CT hours. Funding will also provide provincial programs such as newborn screening, cochlear implants, sexual assault and domestic violence centres.
- Supporting Hospital Beds: Funding to support hospitals expanding services and updating equipment and facilities. Funding will also support newly opened reactivation care centres, which provide temporary care to help patients who no longer need acute care services and are waiting for alternative care facilities, such as long-term care homes.
- Providing Clinical Services: additional funding to emergency departments and support services such as obstetrics, pediatrics, ambulatory care medicine and hospital-based mental health.
- Specialty Psychiatric Hospitals, Specialty Children Hospitals and Small Hospitals: additional funding for Ontario’s 66 small hospitals, two specialty children hospitals and four specialty psychiatric hospitals.
Addressing the Financial Stability of Public Hospitals
Hospitals have faced unprecedented costs as they continue to respond to the COVID‑19 pandemic, ensuring that the people of Ontario have access to the care and treatment that they require. This is why Ontario is providing approximately $700 million in additional financial assistance to public hospitals across the province. This funding for working funds deficits will support eligible public hospitals, with a focus on small and medium hospitals as well as specialty and rehabilitation hospitals that carry a large financial strain due to their unique situations and funding challenges.
These investments will ensure hospitals can continue to provide high-quality patient care that the people of Ontario need and deserve.
Building, Expanding and Improving Hospitals
Ontario is committed to its comprehensive plan to build a health care system that puts patients first. The province’s capital plan includes an investment of $30.2 billion over the next 10 years, including an additional $3 billion since the 2020 Budget, in hospital infrastructure. The government is creating more space for care at this critical time by providing more than $21 billion in capital grants over 10 years to build, expand and renew hospital infrastructure across Ontario. These investments will improve and increase space in hospitals and include grants to support new facilities as well as the renewal of existing hospitals and community health centres.
There are many major hospital projects across Ontario that are currently under construction or in various stages of planning. These projects will help ensure that the people of Ontario have access to the modern facilities and services they need, when and where they need them. In addition, by continuing to invest in health infrastructure renewal, including addressing urgent upgrades through repair and maintenance, Ontario’s health care system will remain sustainable so patients can continue to rely on high levels of care in their own communities.
Ensuring Patients Can Access Vital Blood Products
Plasma is a component of blood used in specialized treatments for a variety of conditions including burns, bleeding disorders, liver diseases and many types of cancer. Some donated plasma is processed into life-saving drugs needed for a variety of rare, life-threatening diseases and genetic conditions.
Ontario is investing an additional $234.9 million over three years to ensure patients can access vital blood products — particularly plasma. Ontario is planning to open an additional six dedicated plasma collection sites to sustain the demand for these vital blood products.
Supporting Specialized Cancer Treatment Services
Ontario is improving access to specialized cancer treatment by supporting the Chimeric Antigen Receptor T-Cell (CAR T) Therapy provincial program. CAR T Therapy is a specialized treatment for pediatric and adult cancer patients with certain types of leukemia or lymphoma, who have not responded to conventional therapies. This specialized treatment is being provided at the Hospital for Sick Children, Juravinski Cancer Centre - Hamilton Health Sciences, Princess Margaret Cancer Centre, and the Ottawa Hospital.
Preventing and Controlling Infections
The Infection Prevention and Control (IPAC) Hub program, launched in fall 2020, helps congregate living settings such as long-term care homes, retirement homes, residential settings for adults and children, shelters and supportive housing, to quickly access IPAC expertise. This helps prevent and respond to disease outbreaks in these settings by making more IPAC resources available.
Since the beginning of COVID‑19, Ontario has invested over $100 million in dedicated IPAC funding, including a significant increase in capacity and measures for both prevention and response. Building on this investment, Ontario is investing $50 million in 2021–22 to ensure IPAC resources and expertise are available across the health system including hospitals and public health units as well as other congregate settings. IPAC provides guidance to prevent the transmission of infections in health care and other congregate settings between residents, staff and other contacts. This vital work protects patients, clients and staff from infectious diseases and viruses, including COVID‑19.
Serving Children with Special Needs
Ontario is ensuring that children and youth with special needs receive the quality treatment they deserve, and that families are supported in navigating their child’s care. This is why the government is continuing to make substantial investments to support new treatment centres for children across Ontario that aim to reduce wait times and meet an increasing demand for children’s services.
Making Record Investments to Address Mental Health and Addictions Challenges
We appreciate the attention that the provincial government has given to the wide‐ranging implications of the pandemic and the support offered to mitigate the stress that it has caused.
Beth Mitchell
Chief Executive Officer
Canadian Mental Health Association
Elgin-Middlesex (CMHA-EM)
Now more than ever, the province recognizes that mental health is health. The COVID‑19 pandemic has intensified the need for mental health and addiction services. More individuals are reporting negative mental health concerns, including anxiety, depression and addiction during COVID‑19, due to business closures and job loss, increased health risks, disruption in schooling and social isolation. The people of Ontario can count on getting the support they need for mental health and addictions challenges.
With the launch of the Roadmap to Wellness in March 2020, Ontario is building a modern and connected mental health and addictions system that makes high-quality services available for people throughout their lifetime, where and when they need them. The Roadmap to Wellness is focused on improving quality, expanding existing services, implementing innovative solutions and improving access. Ontario will provide additional funding of $175 million in 2021–22 for more mental health and addictions support services. This is part of Ontario’s historic investment of $3.8 billion over 10 years for mental health and addictions services.
To deliver on the Roadmap to Wellness, Ontario is implementing a framework to identify and define the core mental health and addictions services to be made available to the people of Ontario, regardless of where they live. This will make it easier to connect providers across community, primary care and acute care settings.
Providing Mental Health Supports for Postsecondary Students
To help postsecondary students during COVID‑19, Ontario has provided an additional $7 million in 2020–21 to increase access to mental health and addiction services, building on an investment of $19.25 million announced in October 2020. This funding will provide services to those studying on campus or virtually and will help address the needs of vulnerable and diverse groups, such as Indigenous students, LGBTQ+ students and students with disabilities.
Assisting People in Crisis
When a person experiences a mental health crisis, police officers are often the first to arrive and offer assistance. This is why Ontario is investing $8.4 million over three years in a crisis call diversion program. This program will offer immediate support for individuals experiencing a mental health crisis, ultimately providing the right supports, which may include diversion to appropriate mental health services. Mental health workers will be embedded in Ontario Provincial Police (OPP) communications centres to provide support to individuals facing a mental health crisis, offer referrals and help people find and access existing services.
Looking Out for Ontario Provincial Police Officers
Ontario recognizes the resolve and dedication of heroic OPP officers, especially during the COVID‑19 pandemic. This is why Ontario is investing $12.5 million over three years to enhance the mental health services available to OPP staff. This initiative is part of Ontario’s response to recommendations made in the Ontario Provincial Police Independent Review Panel: Final Report to create a healthier, more supportive work environment for OPP officers and civilian staff. While the OPP look out for the people of Ontario, they can count on their government to look out for them.
Supporting Ontario’s First Responders
Ontario recognizes the importance of breaking down barriers for first responders in accessing treatment for post-traumatic stress disorder (PTSD) and other mental health disorders. The Province’s investments will work towards both the prevention of PTSD in first responders through early intervention and the return to a healthy and productive work and family life for many.
Helping Our Veterans
In 2020, the government introduced legislation to renew the Soldiers’ Aid Commission and make its support available to more veterans than ever before. Building on this commitment to support those who served our country and their families, the government will be making investments to support veterans’ mental health and their transition to employment through the True Patriot Love Foundation.
Building an Innovative and Responsive Health Care System
A key part of Ontario’s plan to improve the patient experience and support better access to health care services was the creation of Ontario Health Teams and Ontario Health. Ontario Health Teams bring together health care providers to work as one team to improve patient outcomes, with better care coordination and 24/7 navigation of services.
Ontario Health Teams will play an essential role in supporting the government’s priority to deliver a new model of care that will better support patients throughout their entire health care journey. Ontario Health Teams strengthened the local response to COVID‑19 through on-the-ground partnerships in infection prevention and control, testing, isolation centres and staffing support for congregate care settings.
The strong partnerships and integrated care established by Ontario Health Teams and Ontario Health have helped better position the province to respond quickly and effectively to COVID‑19. This includes supporting long-term care homes, simplifying the purchase of PPE, helping establish assessment centres, launching virtual urgent care initiatives and expanding remote patient monitoring programs to support COVID‑19 patients and other vulnerable populations.
Modernizing Home and Community Care for Families
Keeping people in the homes they love, longer, is an important objective for this government. To this end, home and community care plays a vital role in the lives of 700,000 families each year.
The services support people of all ages who require care in their home, at school or in the community. This enables many people living with complex medical conditions to stay in their home. The modernization of Ontario’s home and community care system is necessary to unlock the innovation required to improve services that patients, caregivers and service providers require to make the system more connected to the services that patients need.
Ontario’s plan to modernize home and community care will expand services through investment and additional staff, including PSWs. The Connecting People to Home and Community Care Act, 2020, introduced last year, integrates home and community care into broader health system legislation and recognizes that home and community care is a vital part of an integrated health care system and no longer a stand-alone service. Once proclaimed into force, this new legislation will ensure that home care becomes an essential part of service delivery within Ontario Health Teams, directly connecting patients to the various types of care they need and helping them navigate the health care system on a 24/7 basis.
Supporting Groundbreaking Research in Health Care
Ontario is committed to supporting groundbreaking research to advance new discoveries and innovation, foster a skilled labour force and promote new business opportunities across the province. To support high-value research undertaken in universities, colleges and academic hospitals, the government is investing over $500 million. This will leverage more than $700 million in additional funding from federal, private and other sources over 10 years. This will help strengthen and drive innovation in Ontario with strong partners like the Ontario Institute for Cancer Research, the Ontario Brain Institute, Ontario Genomics, Compute Ontario, and The Fields and Perimeter Institutes.
Protecting Workers
Promoting Workplace Safety
Over the past year, Ontario initiated and implemented a wide range of measures to promote workplace health and safety, protect workers and help reduce the spread of COVID‑19 in workplaces. Ontario is building on these efforts by ensuring that resources are available for employers and workers through initiatives that include:
- Providing free occupational health and safety training for health and safety representatives in up to 60,000 small businesses by investing $3.5 million annually over a three-year period, focused on helping to lower injury rates and improve health and safety awareness and practices in small businesses.
- Releasing an online COVID‑19 safety plan builder that makes it easier and faster for small businesses to develop custom COVID‑19 safety plans that comply with the Occupational Health and Safety Act and the Reopening Ontario (A Flexible Response to COVID‑19) Act, 2020.
- Increasing funding for the Ontario Mine Rescue program by $2.9 million in 2021–22. This funding will include training for underground mining and expand the program’s services to ensure emergency preparedness for all surface and sub-surface mines in the province.
- Renewing the occupational health and safety strategy for 2021 to 2026 to improve health and safety in workplaces, prevent workplace injuries, illnesses and fatalities in the medium and long term, as well as support workplaces through the COVID‑19 pandemic in the short term.
- Supporting Ontario’s Safe Employers, a voluntary program to promote health and safety and reduce injuries and illness in the workplace by encouraging employers to implement an accredited occupational health and safety management system, and conduct hazard and risk assessments.
Keeping Schools Safe
Improving Ventilation and Air Quality in Schools
Ontario continues to take action to ensure school staff and students are safe today and well into the future. Through the 2020 Budget, Ontario led the nation in investments to safely reopen schools by making $1.3 billion in resources available to school boards. Further to these historic supports, the Ontario government is providing an additional $381 million, through the federal Safe Return to Class Fund, including investments of $50 million for HEPA filters and other immediate measures to optimize air quality and ventilation. This investment builds on the $50 million that was announced in August 2020 for improved ventilation and air quality, as well as investments in HVAC and system improvements that will be supported by up to $700 million through the COVID‑19 Resilience stream as part of federal–provincial Investing in Canada Infrastructure Program (ICIP) funding.
Increasing Access to Safe and Affordable Housing
Supporting Housing Stability and Engaging the Federal Government on Housing Supports
Access to safe and affordable housing is a main predictor of well-being for people and families, including improved health and financial outcomes. The COVID‑19 pandemic has had a significant impact on some of Ontario’s most vulnerable, including women fleeing violence and people with developmental disabilities. This is why Ontario is making strategic investments to increase access to safe and affordable housing and provide supports to people experiencing homelessness during COVID‑19, including:
- $255 million in new provincial funding, which was provided to municipal service managers and Indigenous program partners to immediately respond to rising COVID‑19 cases in shelter settings. This builds on the $510 million in funding through the Social Services Relief Fund already provided in 2020–21 to ensure the continuity of critical supports for vulnerable households, including rent assistance programs, protection of residents and staff in homeless shelters and creation of longer term housing solutions.
- $18.5 million over three years, beginning in 2021–22, in the Transitional Housing Support Program, to support victims of domestic violence and survivors of human trafficking to find and maintain affordable housing and help them transition to independence.
- $13 million over three years, beginning in 2021–22, to assist more people with developmental disabilities in accessing community housing and expanding the Adult Protective Service Worker program to support them to live independently.
The Canada-Ontario Housing Benefit (COHB) program helps people pay rent in the private market so they can live closer to family, work and school, while freeing up waitlists to make it easier for others to find community housing. Since launching in April 2020, Ontario has far exceeded its target of assisting 5,000 households through the first year of the program. Ontario is committed to working with the federal government to accelerate the COHB and will continue to seek additional federal funding to assist a greater number of vulnerable individuals access more affordable housing options.
The government of Ontario continues to call on the federal government to provide Ontario with a share of funding under the National Housing Strategy based on its share of households in core housing need. Currently, Ontario is projected to receive $490 million less than its fair share of federal funding over the years of the National Housing Strategy.
Supporting Vulnerable People
Helping Children and Youth with Special Needs
Children and youth with special needs, and their families, have been disproportionately impacted by the COVID‑19 pandemic. School and service closures, as well as other restrictions, have limited children’s access to some services, resulting in delays that can have significant long-term impacts on their health.
To support children and youth with special needs to live happier and healthier lives, Ontario is investing $240 million over four years, beginning in 2021–22. This investment will ensure that more children and families have access to critical services when they need them and build additional service capacity in early intervention rehabilitation and Preschool Speech and Language Program services.
Building Safer Communities
The government continues to listen and take tangible steps to combat systemic racism, including in Ontario’s child welfare system. One of Ontario’s first steps was ending the use of birth alerts, which have an unfortunate history of racial prejudice and discriminatory practices across Canada. The government has also invested $650,000 to support the One Vision One Voice program, a project led by the African-Canadian community to help combat systemic racism and disparities in the child welfare system.
Supporting Victims of Crime
Ontario is committed to standing up for victims of crime and enhancing support services for victims in underserved communities.
Domestic violence has tragically increased during the pandemic. This is why the government provided several investments to combat the impact of COVID‑19 on people and children fleeing violence, including:
- An emergency payment of $2.7 million to help ensure that over 50 community agencies remained accessible to those in need;
- $1 million to help frontline agencies adapt to COVID‑19 remote service delivery and ensure continued operation for the people of Ontario. This funding also supported the operations of the Assaulted Women’s Helpline, including developing text and online chat platforms, setting up toll‑free lines, and providing on-demand interpreter services to respond to increased call volumes; and
- More than $6 million over the next three years to help combat crime and build safer communities from the Proceeds of Crime Frontline Policing Grant. These grants take proceeds from criminal activity and invest it back into communities to help victims, survivors and their families heal.
Building on this support, Ontario is investing an additional $2.1 million over three years to expand victim and sexual assault services in underserved communities, expand free legal support services for survivors of sexual violence across the province, and improve collaboration across the sector to provide seamless supports to victims and survivors.
On February 22, 2021 the Ontario government introduced the Anti-Human Trafficking Strategy Act, 2021, with other new and amended legislation that together support the province’s response to combat human trafficking. Changes include additional supports for survivors seeking restraining orders, including specific consideration for Indigenous survivors, more tools for law enforcement to effectively locate victims and hold offenders accountable, and stronger protections for exploited children.
These initiatives build on Ontario’s support for victims and frontline victim services during the COVID‑19 pandemic and beyond. They are part of this government’s commitment to ensure that victims, survivors and their families continue to get help when and where they need it.
Hiring More Probation and Parole Officers
Ontario is keeping communities safe by investing $23 million over two years to hire 50 additional probation and parole officers. This will help support safe transitions of persons in custody and increase the supervision of offenders to enhance public safety. Through this investment, Ontario will also be increasing community reintegration supports, including gun and gang exit programming, in partnership with municipalities and community organizations.
Supporting Indigenous Women and Girls
Ontario is investing $18.2 million over three years to help address violence against First Nations, Inuit and Métis women and girls. This investment will:
- Enable access to community supports;
- Enhance resources for First Nations police services for sexual assault, human trafficking and domestic violence investigations;
- Provide culturally responsive programming to Indigenous women in the correctional system; and
- Build on existing investments to support community safety and provide additional support to end violence against Indigenous women and girls.
These actions are part of Ontario’s response to the National Inquiry into Missing and Murdered Indigenous Women and Girls.
Addressing Systemic Racism and Hate Crimes
Ontario is committed to collaborating with communities on anti-racism initiatives, as well as increasing public awareness of the impact of systemic racism and hate. This is why Ontario is investing $1.6 million over two years to support the Anti-Racism and Anti-Hate Grant program. This funding will support community-based anti-racism initiatives focusing on anti-Black racism, anti‑Indigenous racism, anti-Semitism and Islamophobia.
This grant program will be developed collaboratively with community partners across Ontario to ensure that it leads to the most effective solutions to fight racism and hate across the province. This builds on Ontario’s previous investment of $60 million over three years for the Black Youth Action Plan to help Black youth achieve social and economic success.
Chart Descriptions
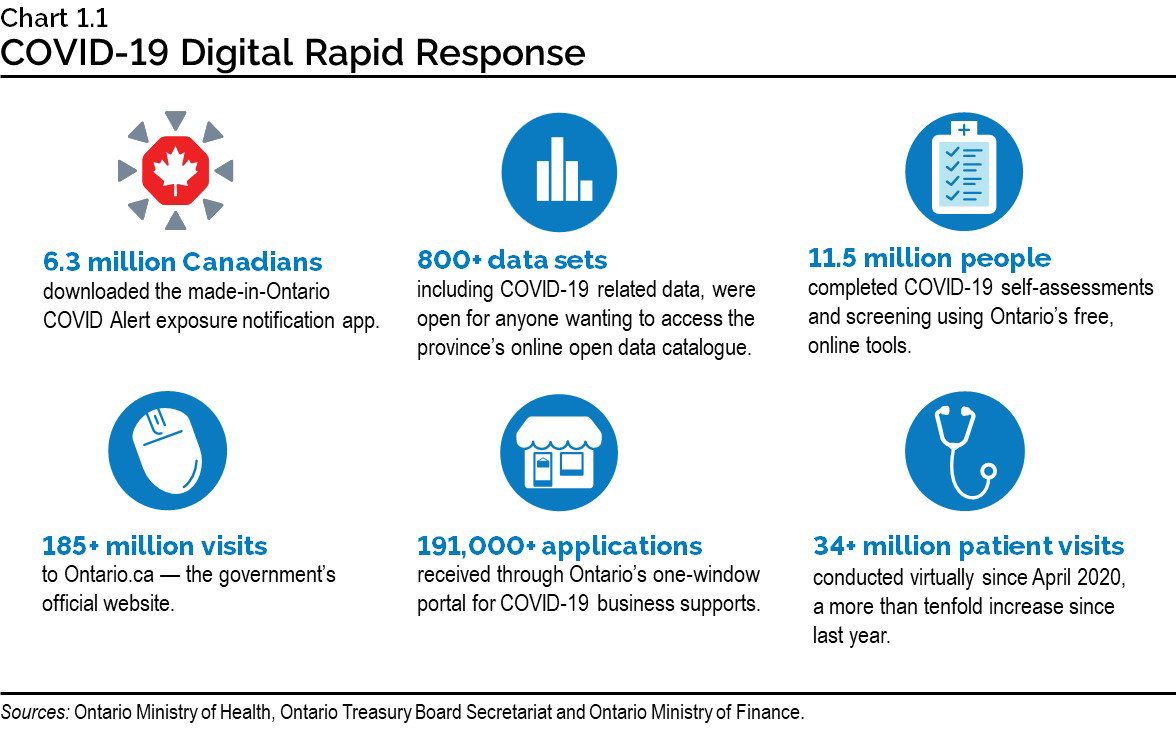
Chart 1.1: COVID‑19 Digital Rapid Response
In the past year, digital and data services helped the people of Ontario navigate these difficult times, access vital information and receive health care and information.
- 6.3 million Canadians downloaded the made-in-Ontario COVID Alert exposure notification app.
- Over 800 data sets, including COVID‑19 related data, were made available for anyone wanting to access the province’s online open data catalogue.
- 11.5 million people completed COVID‑19 self-assessments and screening using Ontario’s free, online tools.
- Over 185 million visits to Ontario.ca —the government’s official website.
- Over 191,000 applications received through Ontario’s one-window portal for COVID‑19 business supports.
- Over 34 million virtual care patient visits since April 2020, a more than tenfold increase since last year.
Sources: Ontario Treasury Board Secretariat; Ontario Ministry Finance; and Ontario Ministry of Health.
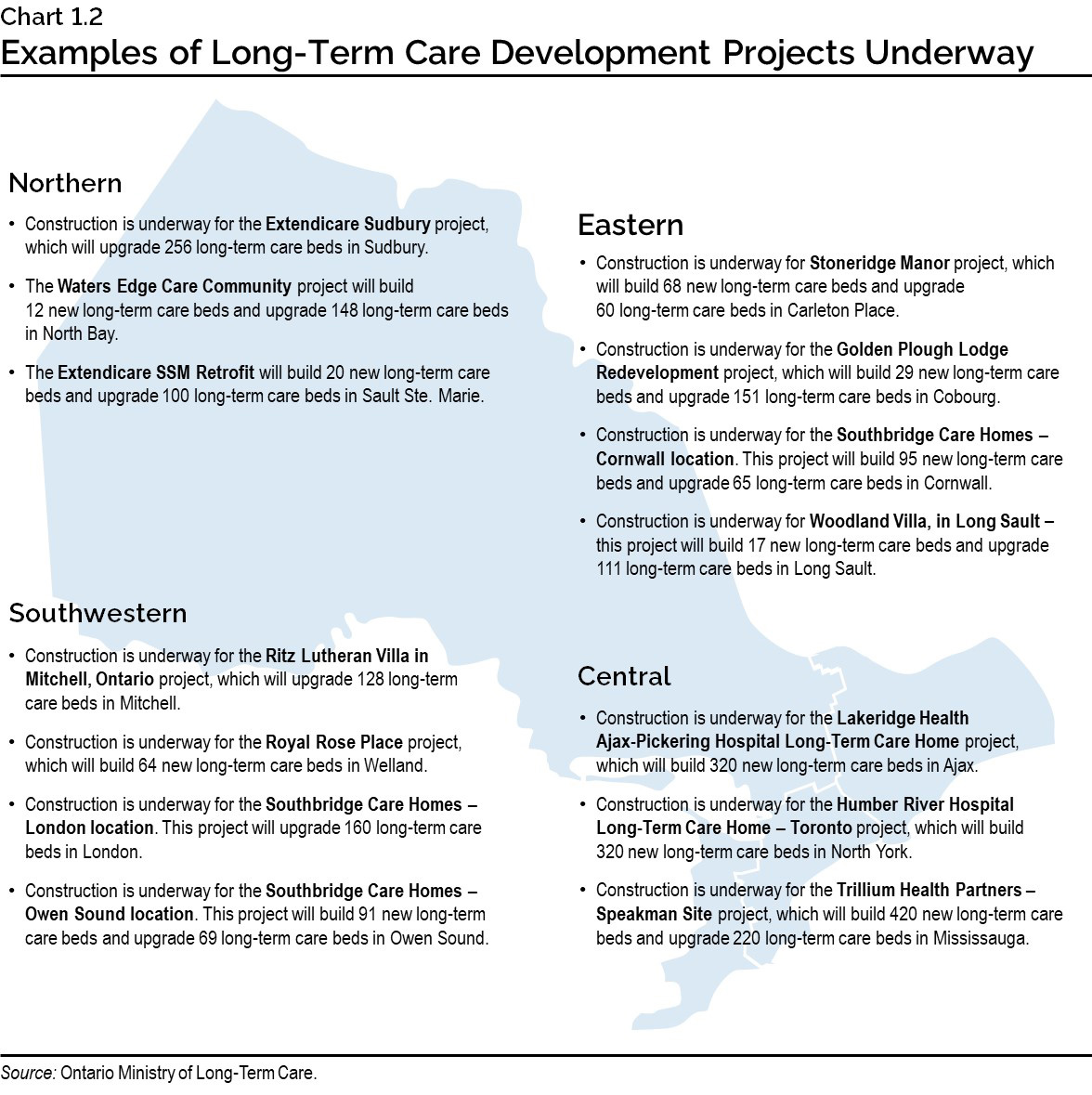
Chart 1.2: Examples of Long-Term Care Development Projects Underway
This map provides examples of long-term care development projects underway across Ontario.
- Northern: Construction is underway for the Extendicare Sudbury project, which will upgrade 256 long-term care beds in Sudbury. The Waters Edge Care Community project will build 12 new long-term care beds and upgrade 148 long-term care beds in North Bay. The Extendicare SSM Retrofit will build 20 new long-term care beds and upgrade 100 long-term care beds in Sault Ste. Marie.
- Eastern: Construction is underway for Stoneridge Manor project, which will build 68 new long-term care beds and upgrade 60 long-term care beds in Carleton Place. Construction is underway for the Golden Plough Lodge Redevelopment project, which will build 29 new long-term care beds and upgrade 151 long-term care beds in Cobourg. Construction is underway for the Southbridge Care Homes — Cornwall location. This project will build 95 new long-term care beds and upgrade 65 long-term care beds in Cornwall. Construction is underway for Woodland Villa, in Long Sault — this project will build 17 new long-term care beds and upgrade 111 long-term care beds in Long Sault.
- Central: Construction is underway for the Lakeridge Health Ajax-Pickering Hospital Long-Term Care Home project, which will build 320 new long-term care beds in Ajax; Construction is underway for the Humber River Hospital Long-Term Care Home — Toronto project, which will build 320 new long-term care beds in North York; Construction is underway for the Trillium Health Partners — Speakman Site project, which will build 420 new long-term beds and upgrade 220 long-term care beds in Mississauga.
- Southwestern: Construction is underway for the Ritz Lutheran Villa in Mitchell, Ontario project, which will upgrade 128 long-term care beds in Mitchell; Construction is underway for the Royal Rose Place project, which will build 64 new long-term care beds in Welland; Construction is underway for the Southbridge Care Homes — London location. This project will upgrade 160 long-term care beds in London; Construction is underway for the Southbridge Care Homes — Owen Sound location. This project will build 91 new long-term care beds and upgrade 69 long-term care beds in Owen Sound.
Source: Ontario Ministry of Long-Term Care.
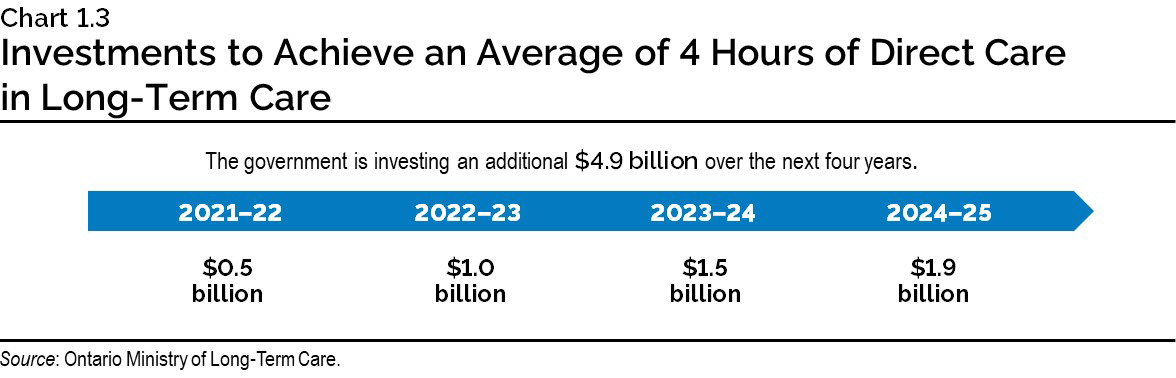
Chart 1.3: Investments to Achieve an Average of 4 Hours of Direct Care in Long-Term Care
This chart illustrates the government is investing an additional $4.9 billion over the next four years including $0.5 billion in 2021–22, $1.0 billion in 2022–23, $1.5 billion in 2023–24 and $1.9 billion by 2024–25.
Source: Ontario Ministry of Long-Term Care.
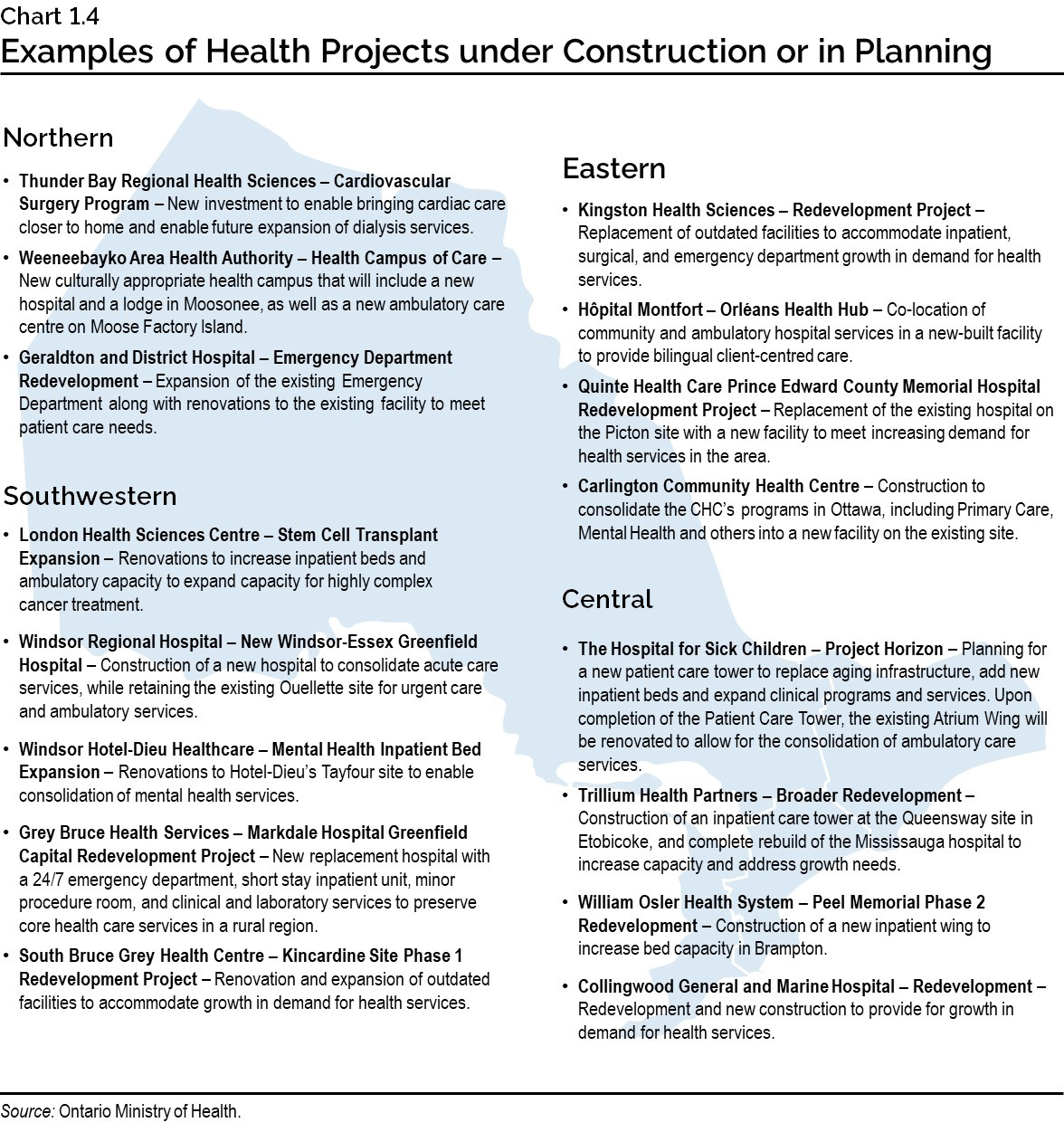
Chart 1.4: Examples of Health Projects under Construction or in Planning
This map provides examples of health facility projects under construction or in planning across Ontario.
- Northern: Thunder Bay Regional Health Sciences — Cardiovascular Surgery Program — New investment to enable bringing cardiac care closer to home and enable future expansion of dialysis services. Weeneebayko Area Health Authority — Health Campus of Care — New culturally appropriate health campus that will include a new hospital and a lodge in Moosonee, as well as a new ambulatory care centre on Moose Factory Island. Geraldton District Hospital — Emergency Department Redevelopment — Expansion of the emergency department along with renovations to the existing facility to meet patient care needs.
- Eastern: Kingston Health Sciences — Redevelopment — Replacement of outdated facilities and accommodate growth in demand for health services. Hôpital Montfort — Orléans Health Hub — Co-location of community and ambulatory hospital services in a new-built facility to provide bilingual client-centered care. Quinte Health Care Prince Edward County Memorial Hospital Redevelopment Project — Replacement of the existing Hospital on the Picton site with a new facility to meet increasing demand for health services in the area. Carlington Community Health Centre — Construction to move the CHC’s programs in Ottawa, including Primary Care, Mental Health and others into a new facility on the existing site.
- Central: The Hospital for Sick Children — Project Horizon — Planning for a new patient care tower to replace aging infrastructure, add new inpatient beds and expand clinical programs and services. Upon completion of the Patient Care Tower, the existing Atrium Wing will be renovated to allow for the consolidation of ambulatory care services. Trillium Health Partners — Broader Redevelopment — Construction of an inpatient care tower at the Queensway site in Etobicoke, and complete rebuild of the Mississauga hospital to increase capacity and address growth needs. William Osler Health System — Peel Memorial Phase 2 Redevelopment — Construction of a new inpatient wing to increase bed capacity in Brampton. Collingwood General and Marine Hospital — Redevelopment — Redevelopment and new construction to provide for growth in demand for health services.
- Southwestern: London Health Sciences Centre — Stem Cell Transplant Expansion - Renovations to increase inpatient beds and ambulatory capacity to expand capacity for highly complex cancer treatment. Windsor Regional Hospital — New Windsor-Essex Greenfield Hospital - Construction of a new hospital to consolidate acute care services, while retaining the existing Ouellette site for urgent care and ambulatory services. Windsor Hotel-Dieu Healthcare — Mental Health Inpatient Bed Expansion - Renovations to Hotel-Dieu’s Tayfour site to enable consolidation of mental health services. Grey Bruce Health Services — Markdale Hospital Greenfield Capital Redevelopment Project - New replacement hospital with a 24/7 emergency department, short stay inpatient unit, minor procedure room, and clinical and laboratory services to preserve core health care services in a rural region. South Bruce Grey Health Centre — Kincardine Site Phase 1 Redevelopment Project — Renovation and expansion of outdated facilities to accommodate growth in demand for health services.
Source: Ontario Ministry of Health.
Chart 1.5: A Fair Federal Share versus the Status Quo
This chart illustrates the gap between a fair federal share (35 per cent) and status quo in Canada Health Transfers (CHT). In 2021–22, this gap represented $28 billion nationally, and $10 billion for Ontario. This gap occurs when CHT as a share of provincial–territorial health spending is 22 per cent rather than 35 per cent in 2021–22. By 2039–40, this gap is estimated to grow to roughly $80 billion nationally, and over $30 billion for Ontario, as the status quo CHT is projected to decline further to less than 18 per cent of provincial–territorial health spending.
Sources: Estimate of provincial–territorial (PT) health costs and status quo Canada Health Transfer (CHT) from PT Finance Ministers report to Council of the Federation (COF) entitled The Canada Health Transfer Will Help Make Provinces and Territories More Financially Sustainable over the Long Term (March 4, 2021); and Ontario Ministry of Finance calculations.